There are four recognized types of Borderline Personality Disorder (BPD), one of which is known as quiet BPD, and it is characterized by internalizing intense feelings of abandonment, shame, and self-blame.
Quiet BPD is lesser known, and many individuals can mask intense emotions. It often differs in its presentation of behaviors compared to typical BPD, however, its approach to treatment is similar. Read on to understand what quiet BPD is, how it differs from other subtypes, and treatment options.
What is Quiet BPD?
Quiet BPD, also referred to as “discouraged BPD” or “high functioning BPD,” describes an individual who internalizes their intense emotions, rather than externalizing them. Like typical BPD, patients with quiet BPD struggle with intense anger, shame, sadness, and guilt. But instead of outwardly displaying it, they often lash out at themselves.
Theodore Millon, a psychologist who specialized in personality disorders, proposed four subtypes of BPD. These include [1]:
- Petulant: “Classic BPD”. A combination of internalizing and externalizing emotions, mood swings, and relationship difficulties.
- Caused by a mix of genetic and environmental factors. Exacerbated by neglect or abuse.
- Discouraged: “Quiet BPD”, emotions are directed inward, social withdrawal, difficulty expressing anger, or being vulnerable
- Linked to experiences of neglect and emotional invalidation, contributing to low self-esteem.
- Impulsive: Poor impulse control, risky or thrill-seeking behavior, sudden mood swings
- Influenced by biological predispositions to impulsivity and lack of control.
- Self-destructive: Self-harm, suicidal thoughts, intense self-hatred, and bitterness
- Often associated with severe trauma or abuse (e.g., childhood sexual abuse)
Of these, the discouraged subtype resembles what many refer to as “Quiet BPD”. Sometimes it is also called high-functioning because individuals can “split off” or mask their intense emotions.
They often appear competent, independent, and in control on the surface, but on the inside experience intense emotional pain. It may appear as social withdrawal, self-criticism, perfectionism, anxiety, and depression.
Recognizing Quiet BPD Symptoms
Quiet BPD is not an official diagnosis recognized by the DSM-5, however, the term is increasingly being recognized to describe the following symptoms, which are often associated with the subtype discouraged BPD [2].
- Intense feelings of anger, shame, sadness, and anxiety, but often directed at the self.
- Avoids conflict, may people-please or repress one’s own needs to make others happy.
- Blame themselves for the conflict or problems.
- Repress anger rather than showing it outwardly, contributing to self-destructive behaviors such as drug use.
- Social isolation due to fear of rejection or when under stress.
- Feelings of low self-esteem, worthlessness, or hopelessness.
- May feel disconnected from themselves, their bodies, or their surroundings, known as dissociation.
- Often able to maintain good work performance, high grades, or outward stability. This can make it difficult to recognize.
BPD Diagnosis Challenges
Stigma, lack of specialized care, and inaccurate self-evaluations play a role in some of the challenges that individuals with BPD face when getting diagnosed. Many individuals with BPD are perceived as crazy, manipulative, or out of control, which can make it more difficult to find treatment, with many clinicians refusing to treat BPD [3].
Other challenges in diagnosis, particularly for those with quiet BPD, include:
- Co-occurring Disorders: BPD symptoms often overlap with other mental health challenges such as PTSD, depression, bipolar disorder, and addiction.
- Internalized Symptoms: Quiet BPD symptoms are often less visible and can be harder to recognize by clinicians and loved ones.
- Fear of Criticism: People with quiet BPD may avoid therapy due to fear of judgment or that they are “unfixable”.
- Diagnostic Gender Bias and Underdiagnosis in Men: Studies have shown a subtle female gender bias in diagnosing BPD. Certain criteria such as “inappropriate and intense anger” are often viewed as more pathological in women, even if men display those traits more frequently [4].
Quiet BPD Treatment: Long-Term Care Approaches
Treatment for Quiet BPD often requires patience, practice, and building a strong therapeutic relationship between the clinician and patient. There are several treatment options for someone with quiet BPD. These include:
- Dialectical Behavior Therapy (DBT): Originally developed to treat BPD, it can help increase distress tolerance, develop self-awareness, and strengthen relationships. It is a first line of treatment for classic BPD, however, those who suffer from quiet BPD and “overcontrol” of their emotions may benefit from RO-DBT.
- Radically Open Dialectical Behavior Therapy (RO-DBT): Focuses on openness, flexibility, and social connectedness to target hidden or indirect sources of loneliness, isolation, and emotional pain.
- Radical Acceptance: Radical self-compassion or radical acceptance is an approach often used in DBT and RO-DBT to help those with quiet BPD cultivate self-kindness and compassion towards their suffering. Compassion-focused therapies have effective results for supporting patients with borderline personality disorder, focusing on helping patients reduce internalized shame and self-soothe [5].
- Creative art therapies: Dance, music, or painting can encourage emotional openness, social connectedness, and help those with Quiet BPD reduce feelings of perfectionism by focusing on the healing artistic journey, not the final product.
Find Hope: BPD Treatment Guided By Empathy at Northbound
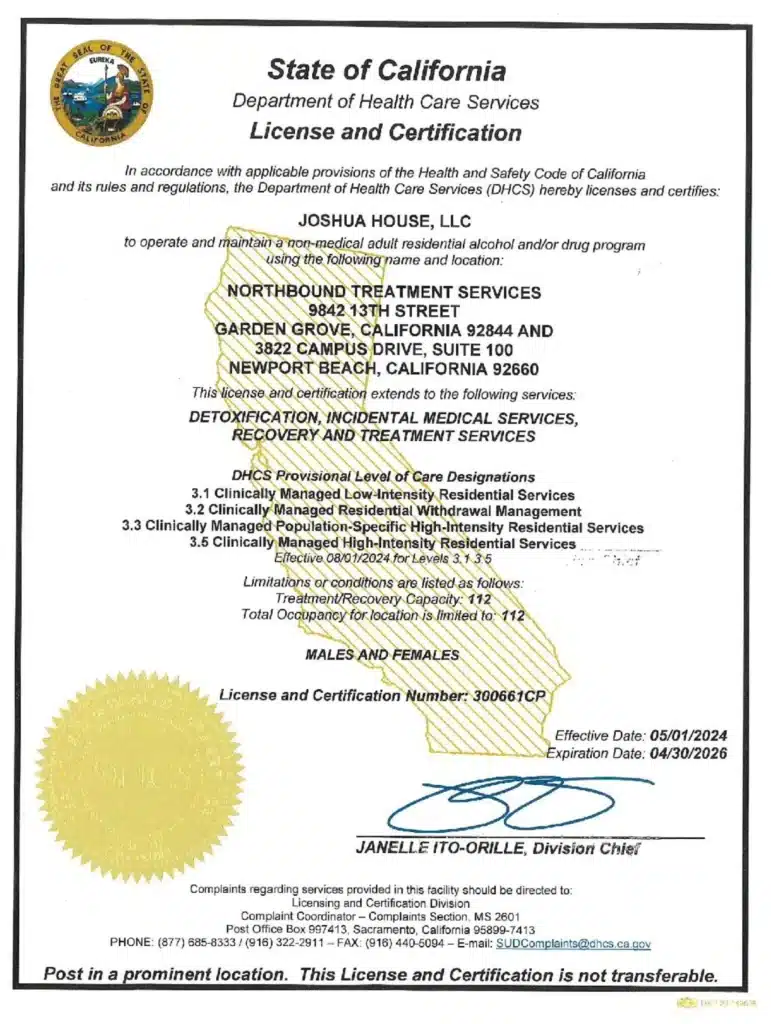
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] NHS. 2025. Causes – Borderline personality disorder.
[2] NHS. 2025. Symptoms – Borderline personality disorder.
[3] Lawn, S. (2022). Structural stigma and its impact on healthcare for borderline personality disorder: a scoping review. International Journal of Mental Health Systems, 16(1), 48.
[4] Soler, J. et al. (2017). Fostering Self-Compassion and Loving-Kindness in Patients With Borderline Personality Disorder: A Randomized Pilot Study. Clinical psychology & psychotherapy, 24(1), 278–286.
Author
-

Clinical Director, Clinical Supervisor, EMDR Provider
I am a Licensed Clinical Social Worker and graduated with a degree from the USC School of Social Work in 2015 with an emphasis in mental health. I began my career working with the Orange County Welfare to Work Program providing mental health services to reduce barriers to employment. I have spent the last 5 years working various levels in behavioral health, providing direct service to those struggling with co-occurring disorders.Using an eclectic and integrative approach, I incorporate the AIP model with EMDR, Person-in-Environment (PIE), Motivational Interviewing (MI), Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), family systems, interpersonal and solution-focused therapy along with Rogerian positive regard into my practice.