Music therapy is a credentialed, clinician-guided service that uses structured music experiences (listening, lyric analysis, songwriting, instrument play) to support goals such as easing anxiety, improving mood, and building coping—always alongside evidence-based care. Evidence shows small-to-moderate benefits for anxiety, mood and engagement, with growing but mixed data in substance use disorder (SUD) [2] [3].
Key Takeaways
- Music therapy complements—not replaces—core treatments (therapy, medication, medical care) [1] [2] [3].
- Benefits supported by research: reduced anxiety or depressive symptoms, better relaxation, pain relief, and higher engagement in care. SUD outcomes are promising but not guaranteed [2] [6] [7] [8].
- Best fit: individuals who benefit from experiential learning and structured coping plans integrated with CBT or DBT (Cognitive Behavioral Therapy or Dialectical Behavior Therapy) [2] [4] [6].
What is Music Therapy?
Music therapy is a clinical service delivered by credentialed professionals (MT-BC) using structured music experiences to meet health goals in hospitals, outpatient clinics, and residential programs. It is designed to complement standard treatments, not replace them [1], [2], [4].
Common Goals
- Anxiety/mood regulation
- Pain management
- Engagement in care
- Skill-building for coping and recovery [2], [3], [4].
Core Methods
- Receptive listening
- Lyric analysis
- Songwriting
- Instrument play
- Guided imagery
- Music—adapted to age, culture, and clinical profile [2], [3], [4.]
How Does Music Therapy Support Rehab & Recovery?
Integration with therapy, medication, and peer support can improve autonomic regulation, attentional control, emotion labeling/processing, and pro-social engagement—skills that generalize to cravings and high-risk moments [3], [4], [7].
Using Music to Help Manage Emotions and Triggers
Tempo, rhythm, and melody can anchor breath work and grounding. Clients practice “music-assisted” distress tolerance they can use outside sessions (e.g., paced breathing with calming music for anxiety) [2], [3], [4], [7].
Craving Management & Cue Reactivity (with CBT/DBT skills)
Within a therapist-guided plan, music pairs with CBT and DBT tools—urge surfing, stimulus control, and coping self-talk—to manage cue reactivity; structured playlists and “if-then” coping sequences help before, during, and after triggers [2], [6], [7], [8].
Identity Rebuilding, Motivation and Social Connection
Songwriting and shared music-making can clarify values, strengthen non-using identity, and build social reinforcement—key in early recovery [4], [7], [8], [10].
What Does the Evidence Say?
Systematic reviews and practice guidance show small-to-moderate improvements in anxiety, depression, pain reduction, and relaxation. Music therapy may boost engagement and retention. Evidence for direct SUD outcomes is emerging and should be framed as supportive, not curative [2], [6], [7], [8].
Anxiety and Mood Support
Across medical and behavioral settings, studies report reductions in anxiety and depressive symptoms that can help patients participate more fully in core treatments [2], [6], [7].
Pain Reduction and Stress Biomarkers
Receptive and active interventions can decrease perceived pain and modulate physiologic markers (e.g., heart rate variability, cortisol), aiding relaxation and recovery readiness [2], [7].
Engagement, Adherence, and SUD Outcomes
Music therapy can improve attendance, retention, and treatment satisfaction. In SUD care it shows promise as a supportive activity for craving reduction when combined with evidence-based treatment. [7], [8]
What Do Sessions Look Like?
1) Assessment
Review substance use history; the presence of co-occurring symptoms such as anxiety, depression or trauma; sensory preferences; triggers; and functional goals (sleep, coping, social connection) [2].
2) Interventions
Calming listening with breath pacing; lyric discussion to reframe thoughts; songwriting for values-based coping; drumming for group cohesion; guided imagery and music for safe emotion processing [2], [4].
3) Integration with Core Therapies and Aftercare Planning
Align with CBT worksheets, exposure hierarchies, relapse-prevention. Send clients home with coping playlists and self-monitoring strategies [3], [4], [7].
Dual Diagnosis: Anxiety, Depression and Trauma
In dual-diagnosis care, music therapy supports mood stabilization and anxiety management while clinicians address underlying disorders. It can scaffold exposure work (pre-session regulation) and provide a tolerable path to emotion processing when purely verbal therapies feel overwhelming [3], [4], [7].
ResidentialTreatment: Where Does Music Therapy Fit?
Residential programs schedule music therapy alongside psychotherapy, psychoeducation, nursing, and psychiatry. Goals include arousal regulation, sleep routines, craving management, and social reinforcement with coordinated handoffs to outpatient/alumni care [2], [4].
Meditation & “Healing Frequency”—What’s the Evidence?
432 Hz, alpha-wave music, crystal bowls: Popular for relaxation, but current clinical evidence is limited and mixed. Likely benefits reflect general relaxation and preference rather than special frequency effects. Use safely as a complement, not a substitute for proven care [3], [10], [11].
How to use meditation music safely: Pair with slow breathing (≈4–6 breaths/min), comfortable volume, and trigger-aware track selection. Integrate into coping plans and track what truly helps [2], [3].
Immersion and Experiential Therapies—What’s the Difference?
Credentialed music therapy involves assessment, treatment planning, and outcomes tracking. Non-clinical “sound healing” or generic frequency tracks may relax some people but aren’t substitutes for licensed care [1], [3], [5].
Who Benefits Most?
People with co-occurring anxiety or depression, those who struggle with purely verbal processing, teens/young adults who prefer experiential learning, and anyone seeking structured “music to help with anxiety” within a professional plan may all benefit from music therapy [2], [3], [7].
Contraindications and Safety
Hearing sensitivity & overstimulation: Start with low volume, slower tempos, shorter sessions. Avoid earbuds if irritating [2].
PTSD triggers and content selection: screen for lyrical/musical triggers. Consider instrumental or neutral content. Clients retain control to pause or stop [3], [4].
Mania/psychosis considerations: Calmer tempos and predictable forms are preferred. Monitor sleep and stimulation [2], [3].
Informed consent & preferences: Explain options. Invite culturally-preferred music. Document consent [1], [2].
Getting Started: What to Expect in Week 1
Orientation & baseline measures: Set expectations, review contraindications and collect baseline mood/craving/sleep metrics [2], [4].
Individualized goals & cadence: Agree on 1–3 measurable goals. Plan 1–2 sessions/week plus brief daily home practice[2], [4].
Progress tracking: Use simple 0–10 mood and craving scales, sleep quality, and coping usage to adjust interventions [3], [7].
Costs & insurance
Coverage varies by plan and setting. Ask whether sessions are delivered by credentialed providers (MT-BC), how services are billed, and what alternatives exist if out-of-network [1], [2].
Aftercare: Keeping the Music Going
Home listening plans & community resources: Build relapse-prevention playlists (regulate → refocus → reconnect). Schedule short daily practice, and consider community ensembles or peer groups [2], [4].
Alumni groups & “if-then” playlists: e.g., “If cravings >6/10, play Track A and start urge surfing for 10 minutes,” then share results with your therapist/coach [7].
Should I Choose Music Therapy?
- My goals include anxiety relief, sleep support, or daily coping skill practice. [2]
- I prefer experiential learning (music-assisted CBT/DBT) alongside verbal therapy. [6]
- I have access to credentialed providers and a program that integrates music therapy with evidence-based care. [1]
- I’m open to tracking outcomes and fine-tuning playlists based on results. [3]
FAQs
What is music therapy?
A clinical service provided by credentialed therapists using music experiences (listening, lyric analysis, songwriting, instruments, guided imagery) to meet health goals within a broader treatment plan; it complements, not replaces, standard care [1], [2], [4].
What are the proven benefits?
Research supports reductions in anxiety and depressive symptoms and pain, and improved relaxation and engagement. In SUD care, early findings suggest better coping and retention when added to evidence-based treatment (supports—not guarantees) [2], [6], [7], [8].
Is 432 Hz a “healing frequency” supported by evidence?
Evidence is mixed/limited. If preferred and safe, it may aid relaxation but should not replace proven treatments [3], [10], [11].
How does music therapy fit with anxiety treatment?
It pairs well with CBT or DBT. Breathing with calming music, values-based songwriting, and pre/post-exposure regulation and debrief all support these therapy approaches [2], [6], [7].
What happens in a typical session?
Brief check-in, targeted music interventions, and a debrief linking skills to real-life triggers. Clients leave with practice plans and playlists [2], [4].
Does insurance cover it?
Many accredited programs include music therapy. Verification depends on plan and setting. Speak with our Admissions team to check coverage and options. [1], [2]
Mini Glossary
CBT (Cognitive Behavioral Therapy): Skills-based therapy that targets thoughts/behaviors linked to symptoms [6].
DBT (Dialectical Behavior Therapy): a CBT-derived therapy emphasizing emotion regulation, distress tolerance, and mindfulness [7].
MT-BC: Music Therapist–Board Certified, the standard U.S. credential for clinical music therapists [1].
Guided imagery & music: Structured listening plus imagery to explore and process emotions [4].
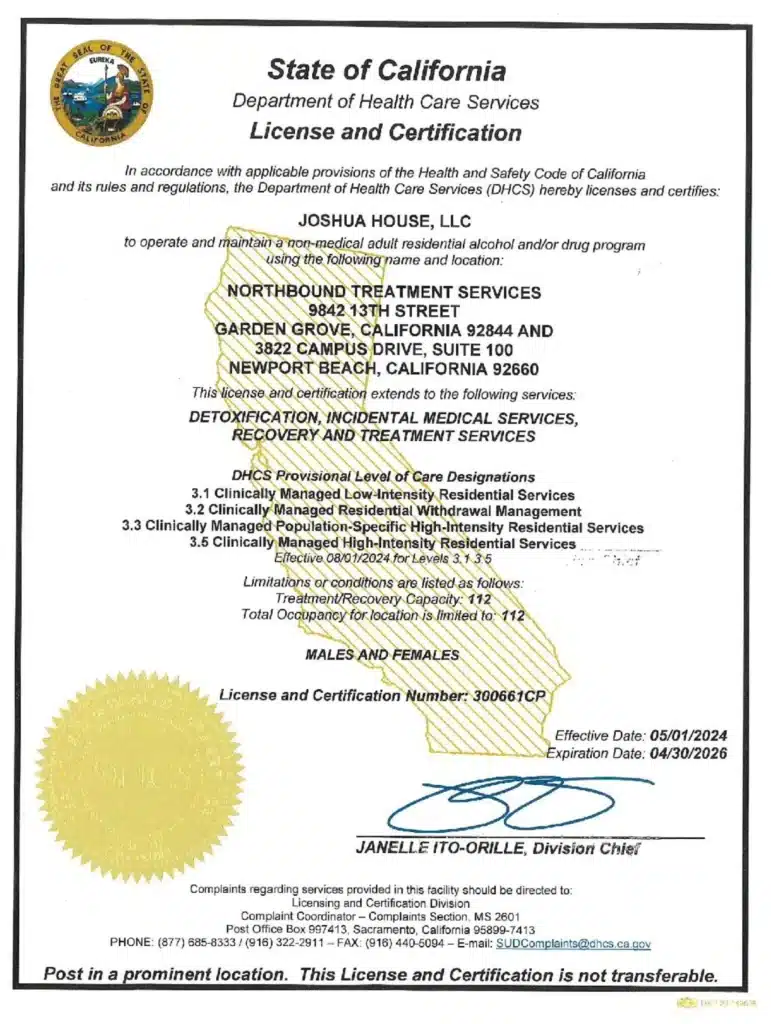
Seeking Help and the Path to Recovery at Northbound
At Northbound, we have extensive experience helping patients overcome their substance abuse addictions.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center for whatever time you may require.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment provides a flexible step-down from our residential program allowing you to live at home and participate for several hours a day.
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
- American Music Therapy Association. (n.d.). Music therapy: FAQ. https://www.musictherapy.org/faq/
- Cleveland Clinic. (2024). Music therapy. https://my.clevelandclinic.org/health/treatments/8817-music-therapy
- National Center for Complementary and Integrative Health. (2024). Music and health: What you need to know. https://www.nccih.nih.gov/health/music-and-health-what-you-need-to-know
- UCLA Health. (n.d.). Music therapy. https://www.uclahealth.org/medical-services/integrative-medicine/music-therapy
- Wikipedia contributors. (2025). Music therapy. Wikipedia. https://en.wikipedia.org/wiki/Music_therapy
- Aalbers, S., et al. (2017). Music therapy for depression. Cochrane Database of Systematic Reviews. https://pmc.ncbi.nlm.nih.gov/articles/PMC5687713/
- Fancourt, D., & Finn, S. (2021). Evidence on the role of the arts in health and well-being. https://pmc.ncbi.nlm.nih.gov/articles/PMC8553721/
- Journal of Substance Abuse Treatment. (2025). Music therapy and SUD: Review/update (pre-proof). https://www.jsatjournal.com/article/S2949-8759(25)00020-7/pdf
- American Psychological Association. (2013). The healing power of music. https://www.apa.org/monitor/2013/11/music
- Ohio University. (2024, July). What makes music therapy effective. https://www.ohio.edu/news/2024/07/what-makes-music-therapy-effective
- PositivePsychology.com. (2024). Music therapy: Definition, types, and benefits. https://positivepsychology.com/music-therapy-benefits/
Author
-

Chief Marketing Officer
Alexa Pelech is the Chief Marketing Officer at Northbound Treatment Services, where she combines her passion for helping others with a strong track record in addiction treatment marketing and outreach. Since joining Northbound in 2019, Alexa has held several key roles—including Referral Relations Manager and Director of Business Development—before stepping into her current leadership position in March 2023.Alexa began her career in behavioral healthcare as an Outreach Coordinator with American Addiction Centers, where she quickly developed a reputation for her compassionate approach and results-driven mindset. Today, she leads Northbound’s marketing strategy with the same energy and heart, driving growth while staying true to the mission of recovery.
Alexa holds a Bachelor of Arts in Fine and Studio Arts from San Francisco State University and later studied Substance Abuse and Addiction Counseling at Los Angeles Pierce College. Her creative background and commitment to service continue to shape her authentic, human-centered leadership style.