Did you know psychosis affects around 3% of people at some point in their lives? [1].
Psychosis and the recovery period typically occur in 5 stages: early or prodromal with subtle changes in thoughts or behavior, acute symptoms where urgent care is required, stabilization where symptoms are managed, recovery with therapy and reintegration into daily life, and life after psychosis, focusing on long-term healing.
Understanding psychosis as a cluster of symptoms rather than a single mental health diagnosis can help guide more effective treatment. Read on to understand more.
What is Psychosis?
Psychosis is a collection of symptoms that affect the mind and essential cognitive functions, causing one to have a loss of contact with reality. During a psychotic episode, one’s thoughts and perceptions are impaired, struggling to recognize what’s real or not. Typical symptoms of an episode of psychosis include [2]:
- Hallucinations: Seeing, hearing, smelling, tasting, or feeling things that are not there.
- Delusions: Strong personal beliefs not shared by others and have no factual basis (e.g., the government is targeting them through a conspiracy).
- Disordered Thinking: Ideas or thoughts occur quickly and may not make logical sense, connect, or flow.
- Other symptoms may include: Paranoia, trouble focusing, decline in work or academic performance, increased anxiety or depression, isolation and social withdrawal, and neglect of self-care.
Types of Psychosis
Psychosis can be caused by a variety of mental health and medical issues. The most common causes are psychotic disorders, a broad category of mental health conditions that present with typical characteristics of psychosis, such as disordered thinking, suspicion, and self-isolation.
Common psychotic disorders and other mental health challenges or medical conditions that can cause psychosis include [2]:
- Schizophrenia: Most common psychotic disorder, characterized by hallucinations and delusions
- Schizoaffective Disorder: Personality disorder characterized by psychotic symptoms combined with mood disorder symptoms such as depression or mania
- Delusional Disorder: Persistent delusions, often involving themes such as persecution
- Substance-induced Psychosis: Triggered by drug or alcohol use, or sometimes withdrawal
- Trauma-induced Psychosis: Comorbid PTSD and psychosis affect around 17% of individuals with trauma
- Stress-induced Psychosis: Triggered by extreme psychological stress (e.g., sudden loss of a child)
- Postpartum Psychosis: Rare, but can be severe and occurs in women after childbirth
- Bipolar psychosis: Symptoms occur during a manic or depressive episode
- Spiritual Psychosis: Experiences interpreted as spiritual or religious visions that may resemble psychosis
- Medical Conditions: Parkinson’s, Alzheimer’s, brain tumors or infections, stroke, MS, epilepsy
Understanding The 5 Stages of Psychosis
For years, psychosis was described as occurring in 3 distinct stages: prodrome, acute, and recovery. However, emerging research claims these are incomplete, and more experts in the field are adopting this view. The five stages of psychosis include:
- Early (Prodrome)
The early stage of psychosis includes subtle changes in behavior such as confusion, memory loss, or saying illogical things. Symptoms can differ from person to person and are not always recognizable, but may include:
- Irritability or aggression
- Feeling depressed
- Hyperactivity
- Neglect of self-care
- Decline in Performance
- Mild hallucinations may begin in this phase
- Acute/Crisis
This is the peak stage of a psychotic episode and often requires immediate medical care, hospitalization, or crisis services. The person becomes absorbed in their inner world and disconnects from loved ones or surroundings.
Symptoms differ from person to person but generally include:
- Distressing, unwanted, extreme, or bizarre thoughts
- Disorientation, mental confusion
- Hallucinations, paranoia, intense anxiety
- Increased risk of self-harm or aggression (can be violent, but this is only in a minority of individuals)
If you or someone you love is experiencing symptoms of acute psychosis, call 988 for immediate mental health support or dial 911 for a medical emergency.
- Post-Acute/Living With Psychosis Vulnerability
This is the brief period immediately following the psychotic episode, but before symptoms have stabilized. The person often feels disoriented and mentally vulnerable. They may also feel guilty or embarrassed. The individual may isolate themselves during this period and begin to process what they just experienced.
- Recovery
During this stage, treatment begins to take effect, and symptoms lessen with support. The individual slowly “returns to the real world” with symptoms like delusions and hallucinations subsiding. Mild symptoms are still present, and individuals may not be able to re-enter their daily routines right away, but the acute psychotic episode is now over.
- Residual/Life After Psychosis
Most symptoms have subsided, and individuals reintegrate into daily life. They may return to daily routines, work, or school, but still struggle with reduced motivation, intrusive thoughts, or anxiety about future psychotic episodes. During this phase, it’s important to continue treatment, focusing on managing symptoms, reducing stress or triggers, and preventing relapse.
Who Can Be Affected By Psychosis?
Studies estimate that between 15 and 100 people out of 100,000 develop psychosis each year. Anyone, from any background, can be affected, and symptoms often first appear in early adulthood (mid-20s) [1].
However, people can experience a psychotic episode at any age, especially if triggered by stress, trauma, or a medical illness. A few groups of people at a higher risk of developing psychosis include:
- Young people aged 14 to 30
- People with a first-degree relative who has experienced psychosis or had a psychotic disorder have a 10% increased risk of experiencing psychosis
- Older individuals with neurological issues
- Those exposed to known risk factors such as trauma, substance abuse, belonging to a minority group, living in an urban environment
How Long Does Psychosis Last?
The prodromal phase (early stage) of psychosis, which includes subtle signs before full psychosis develops, lasts on average about 21 months but can range from 1 to 5 years.
During acute psychosis or a psychotic episode, symptoms such as hallucinations, delusions, and paranoia can vary depending on the person.
Psychotic disorders such as schizophrenia and schizoaffective disorders have symptoms that persist for at least 6 months, often with recurring episodes. Drug-induced psychosis can vary by substance. For example, meth-induced psychosis can last 1 to 6 months, while marijuana-induced psychosis often only lasts a few hours.
Can Psychosis Be Treated? Is There A Cure?
Psychosis can be treated to reduce symptoms, but there is no cure. Treatment usually consists of a combination of medication and therapy.
- Medication: Antipsychotics such as risperidone, quetiapine, and olanzapine are often a first line of treatment for psychosis. These block D2 dopamine receptors, and serotonin 5-HT2A receptors to reduce symptoms within days to weeks.
- Cognitive-behavioral therapy for psychosis (CBT-P): A form of CBT that focuses on socratic questioning to stimulate critical thinking and guided discussions to challenge delusional beliefs [3].
- Psychosocial Interventions such as group therapy, family therapy, and social skills training can complement medication to develop positive coping skills and improve functioning.
Seeking Support? Point Your Compass Northbound
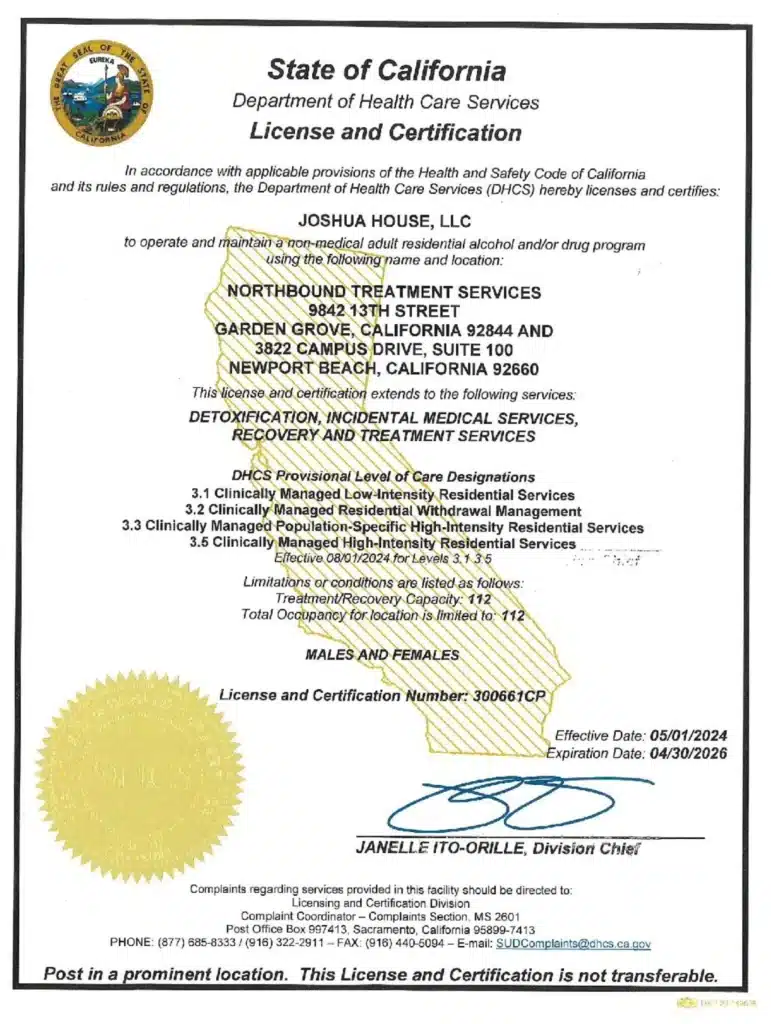
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] NHS. Early Intervention in Psychosis.
[2] National Institute of Mental Health. Understanding Psychosis.
[3] Phiri, P. 2017. A Brief Review of Key Models in Cognitive Behaviour Therapy for Psychosis. Journal of Acta Psychopathologica.
Author
-

Clinical Director, Clinical Supervisor, EMDR Provider
I am a Licensed Clinical Social Worker and graduated with a degree from the USC School of Social Work in 2015 with an emphasis in mental health. I began my career working with the Orange County Welfare to Work Program providing mental health services to reduce barriers to employment. I have spent the last 5 years working various levels in behavioral health, providing direct service to those struggling with co-occurring disorders.Using an eclectic and integrative approach, I incorporate the AIP model with EMDR, Person-in-Environment (PIE), Motivational Interviewing (MI), Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), family systems, interpersonal and solution-focused therapy along with Rogerian positive regard into my practice.