Deciding when and how to do an intervention can be very stressful for loved ones and family members. But it can be very successful when planned well and carried out with integrity and consistency.
Keep the team small, script specific “I” statements, pre-arrange treatment (verify benefits and schedule intake), and set clear, enforceable boundaries. Contingency management (CM) is first-line for methamphetamine use disorder; there are no FDA-approved medications yet [1], [12].
Key takeaways
- Structure a surprise: Plan a private, time-limited meeting—not a public confrontation. [3]
- Act same-day: Verify insurance and book intake before the meeting to cut no-shows and drop-off [9], [10].
- Use proven care: Contingency Management, Cognitive Behavioral Therapy (CBT), and community-reinforcement approaches have strong evidence [1], [7].
- No FDA-approved meds (yet): Medications are under study; behavioral care is first-line [1], [8].
- Safety first: If there’s psychosis, chest pain, seizures, or suicidal intent, call emergency services [1].
What Is a Drug Abuse Intervention?
A drug abuse intervention is a planned, private meeting where a small group shares specific concerns, asks the person to accept help, and offers clear, immediate next steps (e.g., transport to an intake). Goal: reduce harm and connect them to care—today. It’s structured, respectful, and logistics-ready, not a public ambush [3].
How Do You Plan a Family Intervention for Meth?
- Build the team: 2–5 trusted people—family, close friends, sometimes a clinician/intervention specialist. Avoid anyone who escalates conflict. Shared aim: help them accept treatment today. [3]
- Research care: Review credible sources on Meth’s effects and evidence-based care (CM, CBT). Pre-arrange options (detox, residential, outpatient) and confirm admission needs (ID, insurance) [1], [12].
- Write “I” statements & boundaries: Prepare brief, concrete examples of harm.
Boundaries: Set limits you will uphold (e.g., “I won’t provide money or cover bills”) linked to accepting care [3]. - Rehearse the flow: Practice the order, the direct ask (“Please come with us today”), and calm responses to pushback [3]
- Present immediate options (warm handoff): “We verified your benefits; intake can see you at 2 PM. We can drive you.” Warm handoffs and reduced wait times lower no-shows [9] [10] [11].
- Follow through same-day: If they agree, move quickly—transport, paperwork, essentials bag. If they decline, hold boundaries and leave the door open for help later [3].
What To Say (And Not Say)
Best practices
Empathy, specifics, next step: “I’m worried—you’ve lost weight, you haven’t slept, and I found burned foil. We love you. We can take you to rehab today.” Redirect to the plan when conversations drift [3].
Avoid
Blame, empty ultimatums, public scenes. Don’t threaten consequences you won’t enforce [3].
How To Tell If Someone Is On Meth (Signs & Symptoms)
Look for these main visible signs and symptoms.
| Physical signs | Behavioral signs |
| Weight loss | Falling behind on obligations, |
| Dilated pupils | Hyperfocus |
| Skin sores | Rapid/pressured speech |
| Skin picking | Prolonged insomnia and agitation |
| Severe dental issues (“meth mouth”): rampant decay, gum disease, fractures). | Suspiciousness/paranoia |
| Dehydration and teeth grinding worsen dental harm [5] | Risky financial/legal decisions [1] |
What Does “Spun” Mean?
“Spun” is informal slang for being extremely high on meth—often restless, anxious, or paranoid. Use the term only to interpret what someone may mean; it’s not clinical. [7]
Meth Withdrawal, Craving, and Why Timely Treatment Matters
After heavy use, people may “crash” with extreme fatigue, low mood, irritability, and strong cravings. Early, structured support reduces harm and aids stabilization. [1]
Treatment for Methamphetamine Addiction: What Works
Behavioral Therapies
- Contingency Management (CM) therapy provides immediate, meaningful incentives for recovery-aligned behaviors and has the strongest evidence for stimulants. CBT and community-reinforcement help build coping skills and pro-social routines. Combining CM with counseling often improves outcomes [1] [7] [12].
- Medications under study: There are no FDA-approved medications for methamphetamine use disorder; research (e.g., naltrexone + bupropion) shows promise but remains investigational. Behavioral care is first-line treatment [1], [8].
- Family-centered care and aftercare: With consent, involve family. Plan for sleep, nutrition, medical/dental follow-up, and relapse-prevention routines (including CM continuation) [1], [5].
Inpatient vs Outpatient: How Do We Choose?
- When residential/inpatient fits: For psychosis, severe co-occurring disorders, unstable housing, high medical/dental needs, or safety risks that make outpatient attendance unlikely. [1]
- When outpatient fits: Where there is stable housing/transport and support for frequent visits. Pairing with CM improves retention and outcomes [7], [12].
Addressing “Meth Mouth” and Overall Health
- Dental care basics: this may include early evaluation, fluoride, gentle hygiene plans, saliva substitutes, hydration, and coordination between dental and addiction care [5].
- Early recovery foundations: It’s key to normalize sleep, rehydrate, replete nutrition. Treat skin wounds to prevent infection—these basics support therapy engagement [1].
Risks, Safety, and When to Call for Help
- Emergency red flags: If the person shows severe paranoia/psychosis, chest pain, shortness of breath, seizures, or suicidal intent—call emergency services immediately and share substances and timing of known use with responders [1].
- Why urgency matters: Stimulant-involved overdose deaths remain elevated in the U.S. [4].
How Do Families Sustain Change After the Intervention?
- Hold boundaries: Keep limits you set (no cash, no cover-ups). Replace enabling with supportive acts (rides to appointments, shared meals) [3].
- Support recovery structure: Attend family sessions if available, track CM milestones, rebuild daily routines—sleep schedule, meals, chores, school/work tasks [7].
- Know what’s available: Some states are funding CM for stimulant use disorders (e.g., California’s DMC-ODS CM program). Ask programs if they offer CM or can refer you [6].
Costs, Insurance, and Accessing Care Quickly
Verify benefits: Do this before the meeting. Pre-schedule intake and plan transportation. Bring ID and a current meds list.
Why it matters: Shorter waits and warm handoffs reduce no-shows and early dropout [9], [10], [11].
FAQs
How do I know it’s time for a Meth intervention?
If safety, health, work/school, or relationships are deteriorating despite consequences, plan a small, structured meeting with same-day options. [3]
What are early behavioral signs of Meth use?
Short sleep, rapid speech, hyperfocus on tasks, skipping obligations, secretive spending, and growing suspicion or irritability are common flags. [1]
Is there medication for Meth addiction?
No FDA-approved medication exists yet. Behavioral therapies—especially CM—are first-line, with active research on medications [1], [8].
How fast should we move after the intervention?
Same day is ideal. Verify benefits, schedule intake, and have a ride ready to reduce second thoughts and barriers [9], [10].
Glossary
- Contingency Management (CM): Behavioral therapy that reinforces recovery-aligned behaviors with immediate incentives (e.g., vouchers, gift cards) [12].
- Warm handoff: Direct, same-day transition from one provider/setting to another to prevent drop-off [9].
- “Meth mouth”: Severe tooth decay and gum disease associated with meth use [5].
Need Help?
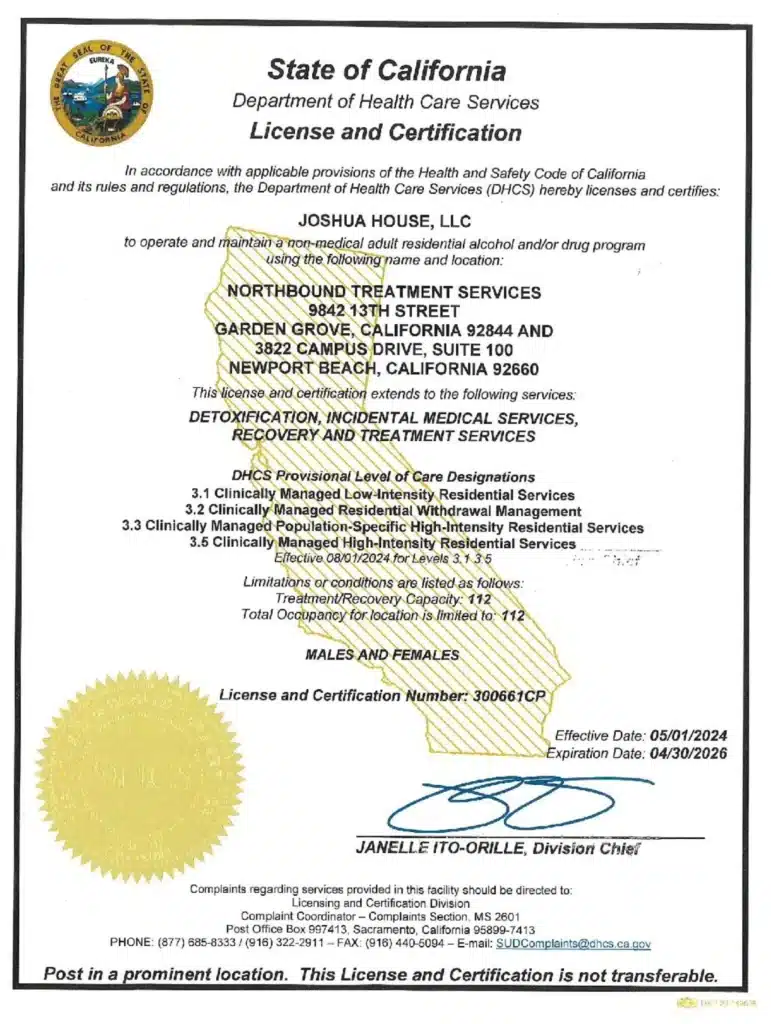
At Northbound, we have extensive experience helping patients overcome their substance abuse addictions, including meth.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center for whatever time you may require.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment provides a flexible step-down from our residential program allowing you to live at home and participate for several hours a day.
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
- NIDA — Methamphetamine: https://nida.nih.gov/research-topics/methamphetamine
- SAMHSA — Helplines (National Helpline 1-800-662-HELP): https://www.samhsa.gov/find-help/helplines
- Mayo Clinic — Intervention: https://www.mayoclinic.org/diseases-conditions/mental-illness/in-depth/intervention/art-20047451
- CDC MMWR — Drug Overdose Deaths Involving Stimulants (Aug 28, 2025): https://www.cdc.gov/mmwr/volumes/74/wr/mm7432a1.htm
- American Dental Association — Meth Mouth: https://www.mouthhealthy.org/all-topics-a-z/meth-mouth
- California DHCS — Contingency Management (DMC-ODS): https://www.dhcs.ca.gov/Pages/DMC-ODS-Contingency-Management.aspx
- De Crescenzo F. et al. (2018) — Network meta-analysis of psychosocial interventions for cocaine/amphetamine use disorders: https://pubmed.ncbi.nlm.nih.gov/30586362/
- NIH (2021) — Naltrexone + bupropion combination shows promise: https://www.nih.gov/news-events/news-releases/combination-treatment-methamphetamine-use-disorder-shows-promise-nih-study
- National Council (2023) — Warm Handoffs for In-Person & Virtual Services: https://www.thenationalcouncil.org/wp-content/uploads/2021/11/Warm-Handoffs-for-In-Person-and-Virtual-Services.pdf
- Molfenter T. (2013) — Reducing appointment no-shows via shorter waits: https://pmc.ncbi.nlm.nih.gov/articles/PMC3962267/
- Pace C. (2018) — Warm Handoffs & attendance at initial behavioral health visits: https://pmc.ncbi.nlm.nih.gov/articles/PMC6037516/
- ASPE/NCBI (2024) — CM evidence & implementation guide: https://www.ncbi.nlm.nih.gov/books/NBK606623/
Author
-

Chief Marketing Officer
Alexa Pelech is the Chief Marketing Officer at Northbound Treatment Services, where she combines her passion for helping others with a strong track record in addiction treatment marketing and outreach. Since joining Northbound in 2019, Alexa has held several key roles—including Referral Relations Manager and Director of Business Development—before stepping into her current leadership position in March 2023.Alexa began her career in behavioral healthcare as an Outreach Coordinator with American Addiction Centers, where she quickly developed a reputation for her compassionate approach and results-driven mindset. Today, she leads Northbound’s marketing strategy with the same energy and heart, driving growth while staying true to the mission of recovery.
Alexa holds a Bachelor of Arts in Fine and Studio Arts from San Francisco State University and later studied Substance Abuse and Addiction Counseling at Los Angeles Pierce College. Her creative background and commitment to service continue to shape her authentic, human-centered leadership style.