Wolf-assisted therapy is a supplemental, clinician-supervised form of animal-assisted therapy (AAT) offered via accredited sanctuaries. Evidence suggests AAT can modestly improve stress, mood, and engagement, but wolves are not service animals under the ADA and these encounters must never replace evidence-based addiction care [4], [6].
Key takeaways
- Add-on, not a replacement: Wolf-assisted experiences should complement—not substitute—detox, medication, or psychotherapy [4], [7].
- Safety and welfare first: Programs must follow infection control, handler certification, and animal-stress safeguards; wolves are never “pets” [5], [7].
- ADA clarity: Only dogs qualify as service animals under U.S. federal rules; wolf/wolf-dog encounters are experiential therapy, not service-animal work [6], [13].
What is Wolf-assisted Therapy?
Wolf-assisted therapy refers to clinician-guided, handler-supervised encounters with wolves or wolf-dogs in accredited sanctuaries and partner facilities as a structured, experiential complement to addiction treatment. Sessions emphasize safe observation, guided interaction, reflective exercises, and therapist-led processing—not ownership or unsupervised handling of wild animals [10] [5].
How Does Animal-Assisted Therapy (AAT) Work in Addiction Care?
Definition: AAT is a goal-directed clinical approach that integrates animals to support therapeutic objectives and engagement [1] [2].
Mechanisms: Potential pathways include reduced perceived stress, increased positive affect, and enhanced treatment participation; evidence quality varies by population and species [4].
Integration: Encounters are woven into care plans alongside Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), trauma-focused therapies, group work, and values/ or spiritual practices where appropriate [3] [4]. Recent syntheses report moderate improvements in anxiety, depression and quality-of-life with AAT in some contexts. Translation to substance use settings should remain conservative and clinician-led [4].
Are Wolves Considered Service or Therapy Animals?
Short answer: No. Under the Americans with Disabilities Act (ADA), only dogs (and in limited cases miniature horses) can serve as service animals; wolves/wolf-dogs do not qualify. Wolf encounters are experiential therapy—not service-animal work or emotional-support-animal access [6] [13].
Comparison of Service vs. Therapy vs. Wolf-assisted
Service animal
What it is: Task-trained dog for disability mitigation
Where it applies: Public access rights under ADA
Who qualifies: Individual with disability
Best for: Ongoing disability support [6]
Therapy animal
What it is: Handler-led visits for therapeutic goals
Where it applies: Facilities/clinics by policy
Who qualifies: Program-screened clients
Best for: Mood, engagement, stress relief [5]
Wolf-assisted
What it is: Sanctuary encounter + clinician processing
Where it applies: Controlled sanctuary/facility only
Who qualifies: Clinically appropriate clients
Best for: Motivation, boundaries, perspective [10]
Who Is a Good Candidate—and Who Should Avoid Wolf Therapy?
Good candidates: Medically stable adults who:
- Can participate in supervised outdoor activities
- Are open to reflective exercises
- Would benefit from work on calmness, boundaries, perspective-taking, and group cohesion [5]
Avoid or use caution: With individuals who:
- Are in acute withdrawal (detox)
- Have unstable psychosis
- Have severe animal phobia
- Have contraindicated medical conditions; clinicians must screen for risks to both patients and animals [7], [8]
What Happens In a Session?
Checklist (bring/know):
- Clothing: Closed-toe shoes; weather-appropriate layers
- Health: Disclose allergies/immunosuppression
- Mindset: Follow handler cues; no sudden movements; no food/scented items [7]
Typical Process:
- Briefing: Goals, rules, biosecurity, and body-language basics are reviewed by clinicians/handlers [7]
- Guided observation/encounter: Controlled proximity with clear boundaries. Animals’ stress signals prioritized [5]
- Therapist-led processing: Link experience to mindfulness, nonverbal communication, trust, boundary-setting, and values
- Reflection activities: Journaling, small-group processing, or faith-aligned reflection as clinically appropriate [10]



How Much Does It Cost and Will Insurance Cover It?
Clinics typically bill AAT under psychotherapy or rehabilitation codes rather than a dedicated “animal therapy” benefit. Wolf-assisted programs may involve separate sanctuary and handler costs. Coverage varies by plan and medical necessity. Verify benefits with the provider before scheduling [8] [10].
How to enroll:
- Step 1: Call admissions to verify benefits and ask about any facility/sanctuary fees [10]
- Step 2: Request your personalized treatment plan and where wolf sessions fit
- Step 3: Obtain written safety/welfare protocols (patient + animal)
- Step 4: Schedule trial session + set measures (mood and craving scores) to track outcomes
How Do Programs Protect Safety, Ethics, and Animal Welfare?
Standards: Programs should follow infection-control, handler certification, animal-stress thresholds, and emergency procedures consistent with federal/VA guidance for animal-assisted interventions) [5] [7].
Bottom line: Wolves are not pets. Ethical programs balance therapeutic goals with animal welfare and client safety at all times.
Aftercare: How Do You Turn Insights Into Recovery Skills?
Convert the experience into skills:
- Grounding plan: 2–3 breath or sensory drills for high-arousal moments
- Boundary scripts: “If X happens, I will do Y”
- Relapse-prevention micro-plan: Triggers → early-warning signs → first aid steps → support call list
- Trust-building reps: Short, repeated commitments that rebuild confidence
First-week plan:
- Day 1–2: Journal insights; share with clinician/peer group
- Day 3–4: Practice one boundary script in a low-stakes setting
- Day 5–7: Pair mindfulness under stress with a routine (walk, meeting, prayer). Re-score mood and cravings
FAQs
Is there proof that wolf therapy works?
Evidence for AAT overall is growing (with dogs and horses most studied). Wolf-specific data are limited, so treat it as supplementary alongside established addiction treatments [4] [12].
How many sessions are typical?
Your clinician will determine frequency within a broader plan (e.g., CBT/DBT groups, individual therapy). Consistency and safety protocols matter more than session count [1], [4].
Is wolf therapy a substitute for medical detox?
No. Detox and stabilization require medical supervision. Experiential therapies may enhance motivation and insight but must not supplant core clinical care [5], [7].
Does insurance cover wolf therapy?
Coverage depends on your plan and whether the service is billed under psychotherapy plus any sanctuary/handler fees. Verify benefits with admissions before booking [8] [10].
Mini Glossary
- Animal-assisted therapy (AAT): Goal-directed clinical use of animals to support health outcomes under professional supervision [1].
- CBT (Cognitive Behavioral Therapy): Skills-based therapy to change thoughts/behaviors linked to cravings and relapse.
- DBT (Dialectical Behavior Therapy): Therapy emphasizing distress tolerance, emotion regulation, and mindfulness—useful for recovery skills.
- Service animal: ADA-recognized dog trained to perform tasks for a person with a disability [6].
- Therapy animal: Handler-guided animal used in therapeutic settings without ADA public access rights [5].
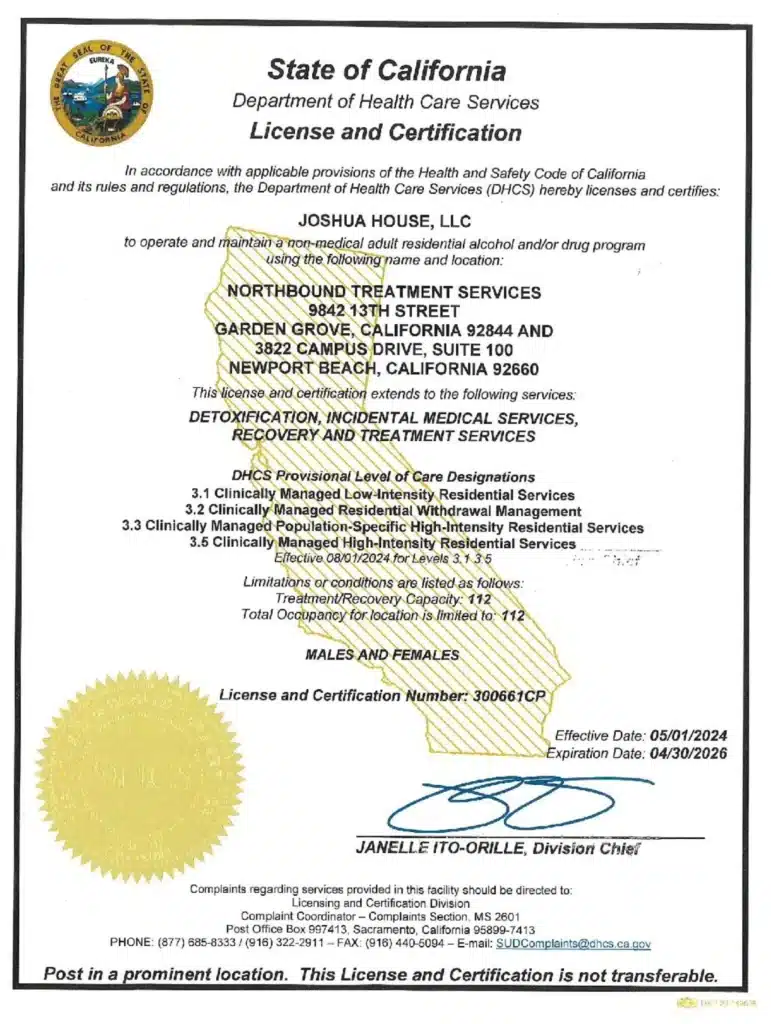
Seeking Help and the Path to Recovery at Northbound
At Northbound, we have extensive experience helping patients overcome their substance abuse addictions.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center for whatever time you may require.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment provides a flexible step-down from our residential program allowing you to live at home and participate for several hours a day.
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
- Psychology Today — Animal-assisted therapy: https://www.psychologytoday.com/us/therapy-types/animal-assisted-therapy
- Wikipedia — Animal-assisted therapy: https://en.wikipedia.org/wiki/Animal-assisted_therapy
- Medical News Today — Animal therapy overview: https://www.medicalnewstoday.com/articles/animal-therapy
- JMIRx Med (2024) — Systematic evidence on AAT: https://pubmed.ncbi.nlm.nih.gov/38606668
- U.S. Department of Veterans Affairs — Whole Health: AAT: https://www.va.gov/WHOLEHEALTHLIBRARY/tools/animal-assisted-therapies.asp
- ADA.gov — Service animals (requirements): https://www.ada.gov/resources/service-animals-2010-requirements/
- VHA Directive 1178(1) (2024) — AAI/AAI services: https://www.va.gov/VHAPUBLICAtIONs/ViewPublication.asp?pub_ID=11704
- Verywell Health — What is animal therapy?: https://www.verywellhealth.com/animal-therapy-5212800
- Husson University — Benefits of AAT: https://www.husson.edu/online/blog/2022/07/benefits-of-animal-assisted-therapy
- Northbound Treatment — Wolf-Assisted Therapy: https://www.northboundtreatment.com/wolf-assisted-therapy/
- OSU Wexner — Buckeye Paws program: https://wexnermedical.osu.edu/features/buckeye-paws-program
- News-Medical — AAT impact; research needs: https://www.news-medical.net/news/20191218/Animal-assisted-therapy-could-have-substantial-impact-on-peoples-health-but-more-research-is-needed.aspx
- ADA National Network — Service vs. emotional support animals: https://adata.org/guide/service-animals-and-emotional-support-animals
Author
-

Program Director
Amanda has been working in the behavioral healthcare field since 2011. During her career, she worked her way through various positions in behavioral healthcare and finally earned a position as a program director over 10 years ago. Amanda initially graduated with her license in vocational nursing and an associate degree with completed certifications in substance use and abuse. Amanda has continued on in her education, and she obtained her bachelor’s degree in the science of nursing obtaining a BSN, and her RN licensure. With a primary background in nursing and medical care, and a proven track record in leadership positions in Behavioral Healthcare, Amanda is the perfect person to manage the daily medical and clinical services of a healthcare treatment facility.
As the Executive Director of Northbound, she utilizes her personal recovery experience coupled with her professional experience to oversee the clinical, medical, and the overall operational function of the organization. She believes that above all else the quality of client care should be the top priority for all the employees at Northbound. She pushes clients to find passion in recovery and to gain meaningful and impactful messages in the group programming to provide lasting recovery.
Amanda has a 17-year-old son. She has a passion for fitness and enjoys Rock Climbing and backpacking in her free time. Her passion for the outdoors plays a major role in her content creation in the daily programming for the schedule at Northbound.