Pulling a muscle in your back or neck can be agonizing, leading to painful spasms that refuse to subside. All we wish for is relief, and the sooner the better. So off we go to a doctor who prescribes a muscle relaxer, and a few hours later we start to feel better. While these medications can provide welcome relief, it’s important to understand the potential risks.
There are two types of muscle relaxers: antispastics and antispasmodics. Each differs in their uses, how they work and side effects. This article focuses primarily on the more common skeletal muscle antispasmodics, also known as skeletal muscle relaxers (SMRs). In fact, a study of US physician visits showed that prescribing SMRs doubled between 2005 and 2016 [1].
But there’s a double-edged sword to this much-needed relief, as many patients and their loved ones are left wondering: are muscle relaxers addictive? Yes, they can be, but the line between necessary medication and misuse can be blurry, and it’s a common concern. Read on to learn more about SMRs, their effects, and why some can be addictive.
What Are Muscle Relaxers and How Do They Work?
Centrally-acting SMRS such as Cyclobenzaprine (Flexeril), Tizanidine (Zanaflex), and Methocarbamol (Robaxin), work in the brain and central nervous system. They depress the central nervous system by blocking nerve impulses in the brain and spinal cord that are sent to the muscles. This helps reduce muscle spasms.
The SMR Baclofen (Lioresal) works by mimicking the neurotransmitter GABA in the brain and spinal cord, effectively suppressing the signaling of neurons that control muscle tension, which leads to reduced muscle spasms. Together, these are the muscle relaxants with the highest potential for misuse and dependence.
For clarity, there are other OTC products which are often the first-line treatment and don’t require a prescription. While they can help with muscle spasm, they are not muscle relaxers per se and may not have the same effect. They include:
- OTC Pain Relievers and Anti-inflammatories: Ibuprofen such as Advil and Motrin, Naproxen, Acetaminophen such as Tylenol
- Topical Analgesics: Creams, Gels, and Patches
- Magnesium Supplements
Are Muscle Relaxers Addictive?
Yes, certain muscle relaxers have a significant potential for psychological and physical dependence, leading to addiction and Substance Use Disorder. These medications are intended for short-term use (2-3 weeks). Taking them for longer than prescribed is a sign of possible dependence and addiction.
SMRs depress the central nervous system as do alcohol, benzodiazepines, and opioids. Over time, the brain adapts to the drug’s presence. It may stop producing its own “calming” chemicals (like GABA), relying on the SMR to feel normal.
Sought-after effects that can lead to misuse include:
- Feelings of euphoria
- Deep relaxation
- Sedation
- Reduced anxiety
What Are the Risks of Taking Muscle Relaxers?
As there are different risks with different SMRs it’s important to talk with your medical provider or pharmacist about possible side effects. Some of these include [2] [3] [4]:
- Drowsiness and fatigue
- Dizziness
- Headache
- Dry mouth
- Fatigue
- Constipation
- Nausea
Most SMRs are well tolerated. However, there are also more serious side effects, such as fainting and blurred vision, that require a conversation with a medical provider or pharmacist.
What Are the Signs of Dependence and Addiction?
There are no over-the-counter (OTC) muscle relaxers in the US. All require a prescription. So abuse requires various techniques such as doctor shopping, trading food stamps, lying, or theft to obtain more of the drug. These are clear signs of dependence or addiction.
Certain SMRs may be abused due to their various effects, including euphoria. So using them for other than their intended effects, or taking them in excess of the prescribed amounts can lead to psychological dependence and physical addiction.
For some, even when using a drug at the prescribed dose, the body can develop tolerance. As a result higher doses are needed to have the original effect.
The most common SMRs associated with risk of abuse, typically after 2-3 weeks, are [4]:
- Diazepam (Valium). A benzodiazepine medication that is prescribed in this case for its muscle relaxant properties, among others, with great potential for addiction
- Carisoprodol (Soma)
Key signs of a dependence or addiction problem include:
- Tolerance: Needing higher doses to achieve the original effect.
- Using more than prescribed: Taking larger doses or using them longer than directed.
- Cravings and compulsive use: Spending a lot of time obtaining, using, or recovering from the drug.
- Continued use despite negative consequences: Problems at work, in relationships, or with health don’t lead to stopping use.
- Withdrawal symptoms: Experiencing physical or psychological symptoms when stopping.
The Dangers and Risks of Muscle Relaxer Abuse
Factors that increase addiction risk include:
- History of substance abuse
- Taking higher doses/longer than prescribed
- Mixing with other substances (alcohol, opioids)
- Underlying mental health conditions
If you are taking higher than recommended doses or have a history of long-term use and suddenly stop taking the following medications, you may experience withdrawal:
- Baclofen (intrathecal injection)
- Diazepam
- Carisoprodol
Common withdrawal symptoms include:
- Rebound anxiety and insomnia
- Muscle pain and spasms
- Hallucinations
- Seizures
These medications need to be gradually tapered under a doctor’s supervision, to prevent withdrawal symptoms.
Central nervous system depression is a very serious risk associated with combining SMRs and opioids such as oxycodone, morphine or fentanyl. These opioids also have the same effect and combining them is absolutely not advised [4].
As well, benzodiazepines, carisoprodol, and opioids (often referred to as the “Holy Trinity”) are avoided within the same prescription for safety reasons and dangers of abuse.
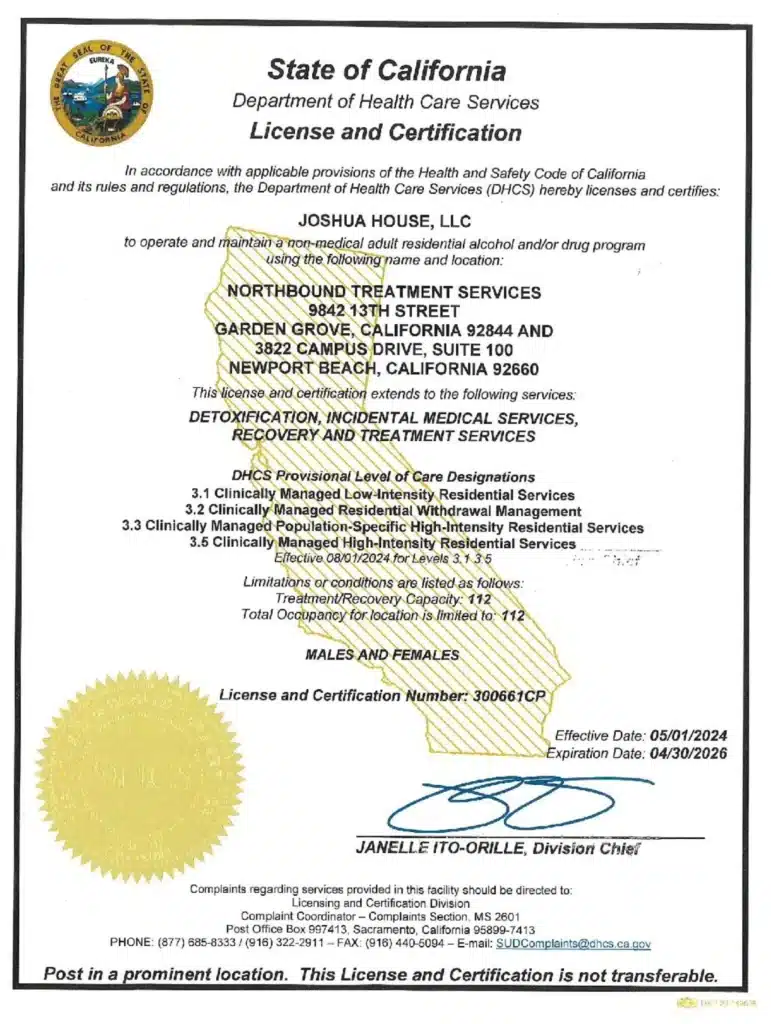
Seeking Help and the Path to Recovery at Northbound
At Northbound, we have extensive experience helping patients overcome their substance abuse addictions.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center for whatever time you may require.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment provides a flexible step-down from our residential program allowing you to live at home and participate for several hours a day.
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] Soprano S. et al. 2020. Assessment of Physician Prescribing of Muscle Relaxants in the United States, 2005-2016. JAMA Netw Open. 2020;3(6)
[2] Caporuscio J. 2025. Types of muscle relaxers and potential alternatives.
[3] Cleveland Clinic. 2023. Muscle Relaxers. Clevelandclinic.org
[4] de Falla K. 2023. Side Effects and Risks of Muscle Relaxers. Spine-Health.com
Author
-

Program Director
Amanda has been working in the behavioral healthcare field since 2011. During her career, she worked her way through various positions in behavioral healthcare and finally earned a position as a program director over 10 years ago. Amanda initially graduated with her license in vocational nursing and an associate degree with completed certifications in substance use and abuse. Amanda has continued on in her education, and she obtained her bachelor’s degree in the science of nursing obtaining a BSN, and her RN licensure. With a primary background in nursing and medical care, and a proven track record in leadership positions in Behavioral Healthcare, Amanda is the perfect person to manage the daily medical and clinical services of a healthcare treatment facility.
As the Executive Director of Northbound, she utilizes her personal recovery experience coupled with her professional experience to oversee the clinical, medical, and the overall operational function of the organization. She believes that above all else the quality of client care should be the top priority for all the employees at Northbound. She pushes clients to find passion in recovery and to gain meaningful and impactful messages in the group programming to provide lasting recovery.
Amanda has a 17-year-old son. She has a passion for fitness and enjoys Rock Climbing and backpacking in her free time. Her passion for the outdoors plays a major role in her content creation in the daily programming for the schedule at Northbound.