Nearly 30 million adults in the US report using benzodiazepines such as Xanax. People often mistake Xanax for an opioid due to their similar depressant effects on the central nervous system (CNS) and high risk of addiction. However, these are two entirely different drug classes, prescribed for different health conditions [1].
Xanax is considered a psychiatric medication and is used to treat mental health disorders such as Generalized Anxiety Disorder and Panic Disorder. Opioids are used for chronic pain and musculoskeletal disorders.
Read on to learn more about Xanax, how it differs from opioids, and what to do when Xanax use becomes a concern.
What is Xanax, and What is It Used For?
Alprazolam, sold under the brand name Xanax, is a benzodiazepine medication primarily used to treat anxiety disorders, especially for physical symptoms of anxiety or panic attacks such as increased heart rate, chest tightness, inability to sleep, sweating, and shakiness. It is also prescribed off-label for short-term treatment of other mental health challenges such as fear of flying, insomnia, and trauma-related anxiety.
Xanax works quickly, relieving symptoms in as little as 15 to 30 minutes. It works by binding to and increasing the effects of the neurotransmitter gamma-aminobutyric acid (GABA). This boosts the natural calming and sedating effects of GABA.
Xanax is available in immediate-release tablets that work within 30 minutes but may require multiple doses a day. It also comes in an extended-release version (Xanax XR) for a one-time daily dose. Xanax is a controlled substance with a high potential for abuse, it should only be taken exactly as prescribed under medical supervision [2].
Opioids vs Benzos: Understanding Drug Classes
Opioids and benzos tend to get mistaken for each other as they cause similar sedative effects, and both carry high risks of addiction. However, these are two separate drug classes that work on different receptors in the brain. Some of the key differences between opioids and benzos include:
| Drug Class | Opioids | Benzos |
| Mechanism of Action | These act on opioid receptors to block pain and relax the muscles | Acts on GABA-A receptors in the brain to reduce central nervous system activity |
| Medications | Oxycodone, Morphine, Vicodin | Xanax, Klonopin, Valium |
| Medical Uses | Chronic pain, post-surgery recovery | Anxiety disorders, insomnia, seizures |
| Side Effects & Risks | Drowsiness, nausea, constipation, respiratory depression, high risk of overdose, and death | Drowsiness, dizziness, confusion, memory loss, high risk of overdose when abused or combined with other drugs or alcohol |
| Risk of Dependency | High risk of physical dependence and intense withdrawal symptoms | Similar risk of physical dependence as opioids, especially when misused |
| Controlled Substance? | Yes | Yes |
Is Xaxan Addictive?
Xanax is addictive and the most commonly abused benzo—around 5.3 million individuals in the US report misusing Xanax. And 10% of those are youth and young adults, leading to a rise in what young people online call the “Xandemic” [3].
Xanax enhances the effects of GABA to promote calmness, euphoria, and relaxation. However, the brain can quickly become dependent as it adapts to these effects. Long-term users of Xanax often need higher doses to feel the same impact. This tolerance problem can develop rapidly in users due to the short-acting nature of xanax.
How Much is Too Much?
The prescribed dose of Xanax varies for each patient, based on the severity of anxiety, response to medication, weight, height, and other factors. Xanax is typically prescribed for short-term use (2 to 6 weeks), and many are only recommended to take it out of necessity (e.g., during a panic attack) rather than as a daily mental health medication.
Signs of Xanax Addiction
Xanax addiction can manifest as physical, psychological, and behavioral symptoms greatly decreasing the quality of one’s life.
| Physical | Psychological | Behavioral |
| Drowsiness, fatigue, slurred speech, and lack of responsiveness | Confusion, mental disorientation, memory loss | Decline in academic or work performance |
| Dizziness, blurred vision, and lack of coordination | Mood swings, irritability, and aggression | Neglecting responsibilities, self-care, and hygiene |
| Nausea, vomiting, dry mouth | Lack of motivation, loss of interest in daily activities | Seeking out multiple Xanax prescriptions, “doctor shopping” |
| Headaches or migraines | Increased depression and anxiety | Risky or reckless behaviors such as driving under the influence or unprotected sex |
| Constricted, pinpoint pupils | Intense cravings for Xanax | Secretive, dishonest behavior, lying, manipulation |
What To Do When Xanax Use Becomes A Concern
If Xanax use becomes a problem, recognizing the warning signs in yourself or a loved one is the first step. Notice signs such as increasing doses beyond what is prescribed, inability to stop using, memory loss, cravings, or inability to function in daily life. If you are concerned about Xanax use, here are a few things you can do:
- Speak with your doctor or psychiatrist and let them know how you are feeling. Likely, they will prescribe you an alternative medication with less risk than benzodiazepine.
- Medical Detox: If you are abusing Xanax, it is essential to withdraw safely under medical supervision, rather than quitting cold turkey. Xanax withdrawal can cause intense symptoms, including seizures.
- Inpatient Rehab: Intensive programs with 24/7 support offer medical care, daily therapy, and group support to target the root of Xanax addiction and develop skills to promote long-term sobriety.
- Outpatient Treatment: Lower intensity programs with more flexibility and less medical monitoring. These may be ideal for individuals whose Xanax addiction has not escalated yet or is less severe.
- Behavioral Therapies like Cognitive Behavioral Therapy are clinically supported as an effective treatment for anxiety disorders. CBT can address the negative thought cycles that contribute to anxiety and addiction.
- Holistic Healing Activities, such as yoga, meditation, art therapy, dance, music therapy, and physical recreation, can support recovery from both anxiety and Xanax addiction.
Prescription Drug Addiction Rehab and Treatment
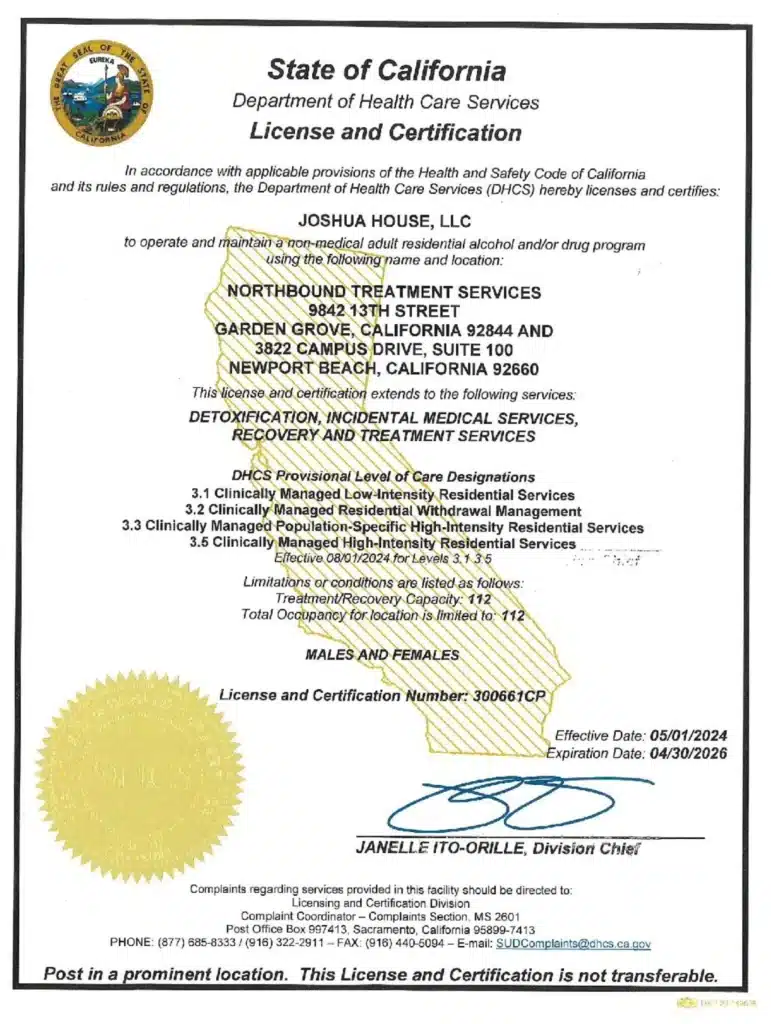
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey from Xanax abuse. Reach out to our admissions team now.
Sources
[1] Low, C. et al. (2019). Benzodiazepine Use and Misuse Among Adults in the United States. Psychiatric services (Washington, D.C.), 70(2), 97–106.
[2] Tobin, G. et al. 2023. Alprazolam. Stats Pearl Publishing. National Library of Medicine.
[3]Surratt, H. L. et al.(2017). Benzodiazepine Dependence among Young Adult Participants in the Club Scene Who Use Drugs. Journal of psychoactive drugs, 49(1), 39–46.
Author
-

Chief Marketing Officer
Alexa Pelech is the Chief Marketing Officer at Northbound Treatment Services, where she combines her passion for helping others with a strong track record in addiction treatment marketing and outreach. Since joining Northbound in 2019, Alexa has held several key roles—including Referral Relations Manager and Director of Business Development—before stepping into her current leadership position in March 2023.Alexa began her career in behavioral healthcare as an Outreach Coordinator with American Addiction Centers, where she quickly developed a reputation for her compassionate approach and results-driven mindset. Today, she leads Northbound’s marketing strategy with the same energy and heart, driving growth while staying true to the mission of recovery.
Alexa holds a Bachelor of Arts in Fine and Studio Arts from San Francisco State University and later studied Substance Abuse and Addiction Counseling at Los Angeles Pierce College. Her creative background and commitment to service continue to shape her authentic, human-centered leadership style.