Many people wonder what the connection is between Suboxone and Methadone for managing Opioid Use Disorder (OUD). They are both used in opioid agonist therapy (OAT) as effective treatments for addiction to opioid drugs such as heroin, oxycodone, hydromorphone (Dilaudid), fentanyl, and Percocet.
These drugs can help people stop or reduce opioid use. They also help treat withdrawal symptoms and reduce drug cravings without creating the strongly pleasurable effects of opioid drugs.
They are long-acting opioid drugs that are used to replace the shorter-acting opioids the person is addicted to. The drug acts more slowly in the body, for a longer period of time, and prevents withdrawal for 24 to 36 hours without causing a person to get high.
Deciding which one works better is really a matter of personalized circumstances and choice. Read on to learn more about this important question.
How Suboxone and Methadone Work
The two drugs have many similarities as described below.
Methadone
Methadone (Methadose) is an FDA-approved Schedule III synthetic, long-term opioid agonist medication. It is used in the management and treatment of opioid use disorder (OUD) within federally regulated opioid treatment programs. Methadone prescriptions are used for both detoxification and maintenance therapy. It is also frequently prescribed to address severe pain associated with cancer and other conditions [1].
Methadone is what is known as a full agonist at the mu-opioid receptor while also affecting other opioid receptors. These mu-opioid receptors are located in different parts of the central nervous system (CNS) and various parts of the gastrointestinal tract. These receptors are key for modulating various neurochemical activities linked to pain management, euphoria, and sedation. Methadone activates the mu-receptors, initiating the same pathways.
Methadone is taken as a drink. Patients must typically attend the Opioid Treatment Program (OTP or clinic) daily to ingest their methadone dose under direct staff observation, especially during the initial phase of treatment (often the first 90 days). A patient can become eligible for take-home doses (carries) by consistently demonstrating stability and compliance.
Suboxone
Buprenorphine (Suboxone) also binds to and activates mu-opioid receptors in the brain, but, as a partial mu-opioid agonist, to a lesser degree than methadone; it also can block other opioid drugs from attaching to those receptors. Like methadone, buprenorphine can reduce cravings and withdrawal symptoms without producing intense feelings of pleasure and intoxication in people who have opioid use disorder.
One of the important characteristics of buprenorphine is the plateauing of its pain management effects at higher doses. As such, it has a ceiling effect on respiratory depression, making it safer compared to methadone in the treatment of addiction [2].
Several buprenorphine products are approved for the treatment of opioid use disorder, including tablets that are placed under the tongue, extended-release injections, and implants. Other products contain buprenorphine together with the overdose-reversal medication naloxone, including tablets or film to put under the tongue or film to place in the cheeks.
Naloxone is added to buprenorphine to reduce the potential for its misuse if someone crushes the tablets and injects it. The absorbed naloxone blocks mu receptors, counteracting the euphoric effects of buprenorphine and potentially inducing withdrawal in opioid-dependent patients.
Buprenorphine alone carries a higher potential for misuse compared to the buprenorphine-naloxone combination.
As of December 2022, the Mainstreaming Addiction Treatment (MAT) Act has eliminated the need for waiver forms by medical practitioners for Suboxone. Those registered with the DEA and holding Schedule III authority are now authorized to prescribe buprenorphine for OUD within the bounds of state law.
This is an important step in making Suboxone more broadly available and increasing the stability, safety, and flexibility of treatment. With this less restrictive prescribing, the so-called “office-based”, flexible model has been made possible.
Comparing Effectiveness and Success Rates in Treatment
Both drugs are highly effective at reducing opioid use. Research shows that Methadone has higher retention rates, likely due to its more structured administration in clinics.
For the same reason, due to its ease of administration in tablet form, Suboxone may have better retention in early recovery, especially if supportive therapy is available. However, some may return to use if their tolerance is very high.
Effectiveness and Safety of Methadone and Suboxone
The following table helps visualize the two drugs [3].
| Factor | Methadone | Suboxone | Key Insight |
| Mechanism of Action | Full opioid agonist. Activates opioid receptors fully, eliminating withdrawal and cravings. | Partial opioid agonist. Activates receptors enough to stop withdrawal and cravings, but has a “ceiling effect. | Methadone provides a stronger effect, which can be critical for high-dose users. Suboxone’s partial effect makes it safer in overdose. |
| Treatment Retention Rates | Generally Higher~60-80% at 6-12 months. | Slightly Lower but High~40-60% at 6-12 months. | Methadone’s structured daily clinic visits contribute to higher retention, especially for those needing more support. |
| Illicit Opioid Use Reduction | Highly EffectiveSuperior at reducing use in highly dependent populations and in first few months. | Highly EffectiveShows similar long-term reduction rates, especially when patient is stabilized. | Both are extremely effective compared to no medication. Methadone may have an edge for more severe OUD. |
| Overdose Mortality Reduction | >50% reduction vs. no treatment. | >50% reduction vs. no treatment. |
Pros and Cons of Each Medication
Which medication is “best” is relative to individual goals, tolerance, and support needs. The “better” option is not about the medication itself, but about which set of practical trade-offs best fits an individual’s lifestyle, needs, and stage of recovery.
This table summarizes the pros and cons of each drug [4]
| Factor | Methadone Pros & Cons | Suboxone Pros & Cons |
| Treatment Structure & Routine | Pro: Provides a highly structured, routine environment with daily contact with healthcare staff. This can be a critical source of stability and support, especially in early recovery. Con: The requirement for daily clinic visits (especially initially) is highly disruptive to work, school, and family life. | Pro: Office-based treatment. Prescriptions can be filled at a pharmacy for take-home use from the start, allowing for minimal disruption to daily life. Con: The lack of daily structure may be challenging for some individuals who need more accountability and support. |
| Access & Availability | Con: Only available at federally regulated and accredited Opioid Treatment Programs (OTPs or “clinics”). These are less numerous, often have waitlists, and may not be available in rural areas. | Pro: Can be prescribed by any waivered physician, nurse practitioner, or physician assistant in a wide variety of settings (doctors’ offices, telehealth). Vastly greater availability and accessibility. |
| Induction risk | Not applicable as it is a full opioid agonist. | Con: Precipitated Withdrawal: Because Suboxone is a partial agonist, if the first dose is taken too soon while full opioids are still on the brain’s receptors, it can forcefully rip them off, triggering immediate and severe withdrawal. |
| Overdose Risk & Ceiling Effect | Con: Unlike Suboxone, there is no ceiling on its respiratory depression effects. This makes it dangerous in high doses or if misused, carrying a significant risk of fatal overdose. | Pro: As a partial agonist, it has a “ceiling effect,” meaning it may not provide enough receptor activation to fully suppress cravings or withdrawal making Methadone a more effective option for these individuals. Con: Less effective for those with a very high tolerance for opioids. |
| Retention & Craving Suppression | Pro: As a full opioid agonist, it stabilizes patients completely, eliminating withdrawal and cravings. This high level of efficacy leads to superior retention rates in treatment programs, especially for those with severe addiction. | Very good, but not as high as Methadone. |
| Dangerous interactions: | Con: Because it has no ceiling effect, its effects are dangerously amplified when combined with other central nervous system depressants like alcohol, benzodiazepines (Xanax, Valium), or sleep aids, drastically increasing the risk of respiratory failure and death. | Con: Suboxone has the same risk factors as Methadone if combined with alcohol, benzodiazepines, or sleep aids. Pro: However, Suboxone’s partial agonist activity and ceiling effect provide a safer pharmacological profile. |
| Stigma & Perception | Con: Carries a high level of stigma. The public perception of “methadone clinics” is often negative. Patients may feel labeled or judged by the community. | Pro: Generally perceived as a more “modern” and less stigmatized treatment. The process of getting medication feels more like standard medical care. |
| Autonomy & Freedom | Con: Significantly less autonomy, especially initially. Earning take-home doses is a slow process (often requiring 90+ days of continuous compliance). Travel is difficult. | Pro: Offers much greater autonomy and freedom from the start. Patients manage their own medication at home, making travel and a normal lifestyle much easier. |
| Treatment Experience | Pro: The clinic provides a built-in community of peers and consistent access to counselors, nurses, and doctors who specialize in OUD.Con: Can feel institutionalizing. Waiting in line daily with other patients can be triggering for some. | Pro: Treatment is integrated into a primary care or psychiatric setting, normalizing the experience. The patient has more privacy.Con: Can feel isolating. The patient must be more proactive in seeking counseling and community support, as it is not built in. |
| Regulatory Hurdles | Con: Heavily regulated by the federal and state governments (e.g., SAMHSA, DEA). Strict rules govern every aspect of treatment, limiting flexibility. | Pro: Prescribed under standard DEA prescribing rules (with a waiver), which are far less restrictive than OTP regulations. Offers more flexibility for the provider and patient. |
| Cost & Insurance | Pro: Often covered by Medicaid and most insurance plans. The clinic model bundles the cost of medication, counseling, and drug testing. Con: The bundled cost can be high without insurance. Daily transportation to the clinic adds a significant indirect cost. | Pro: Covered by most insurance plans and Medicaid. Can be prescribed as a generic, keeping medication cost low. Con: Requires separate payments for the doctor’s visit and the pharmacy prescription. Cost can vary more based on pharmacy and insurance specifics. |
Choosing the Right Fit for Recovery
Choosing the right fit is done with your medical provider, considering a range of factors, among them:
- Severity of OUD
- Tolerance level to opioids
- Medical history
- Insurance coverage
- Availability
- Local regulations
- Need for structure
Methadone is highly effective for severe opioid dependence, including fentanyl and heroin. Abstinence rates from opioid use demonstrate better outcomes when patients undergo long-term rather than short-term methadone treatment.
Methadone has been proven to enhance retention in treatment and detoxification programs, contributing to improvements in mortality rates among individuals with OUDs.Treatment works best when combined with other types of support, such as individual or group counselling [3].
Methadone offers structure and support at the cost of freedom and flexibility. Its model is built around external accountability and is often best suited for environments where that level of support is necessary for stability.
Suboxone offers freedom and autonomy at the cost of built-in structure. Its model is built around integrating treatment into a normal life and requires a greater degree of internal motivation and personal accountability from the patient.
Northbound Treatment’s Approach to MAT
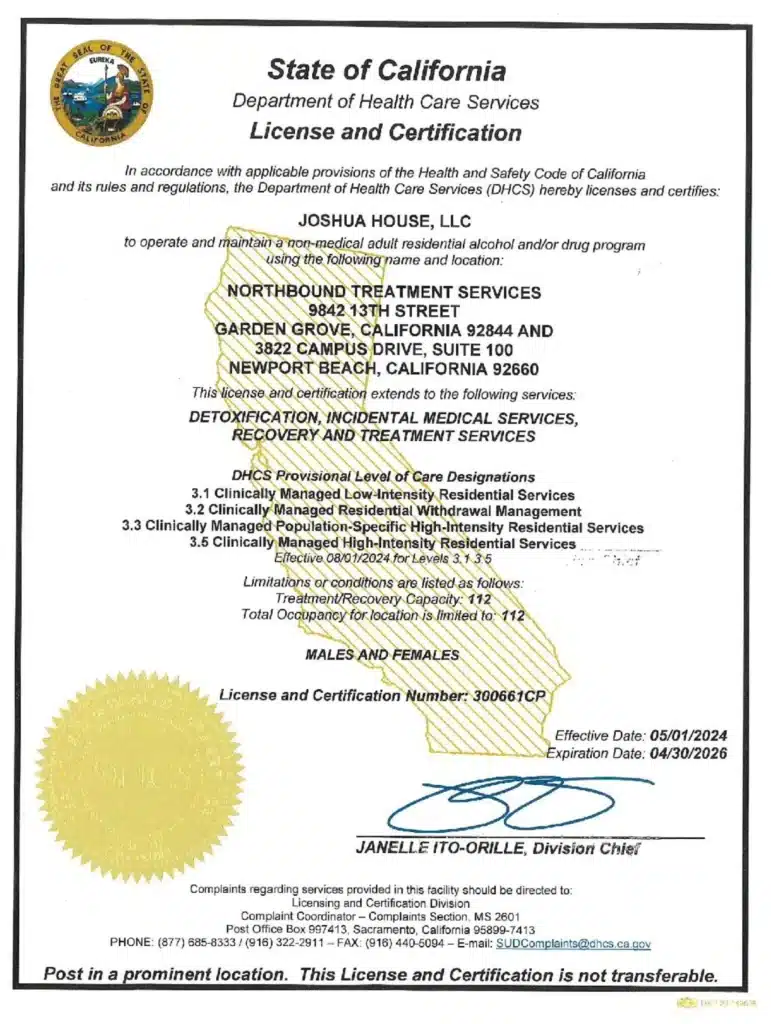
At Northbound we offer a complete Medication Assisted Treatment program, using Methadone and Suboxone. We create a path to long-term sobriety for our patients participating in medical withdrawal management (detox) and treatment for opioids in our program.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center. Opioid agonist therapies such as methadone and buprenorphine are first-line medication-assisted treatments—they relieve withdrawal symptoms, reduce cravings, and can be gradually tapered over time.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment for opioid treatment provides a step-down from our residential program. It offers flexible therapy while living at home.
When it’s Time to Seek Help, Point Your Compass Northbound
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] Durrani M, Bansal K. Methadone. [Updated 2024 Jan 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan
[2] Kumar R, Viswanath O, Saadabadi A. Buprenorphine. [Updated 2024 Jun 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan
[3] Mattick, R. et al. (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. The Cochrane database of systematic reviews, 2014(2)
[4] SAMHSA. 2021. TIP 63. Medications for Opioid Use Disorder.
Author
-

Clinical Director, Clinical Supervisor, EMDR Provider
I am a Licensed Clinical Social Worker and graduated with a degree from the USC School of Social Work in 2015 with an emphasis in mental health. I began my career working with the Orange County Welfare to Work Program providing mental health services to reduce barriers to employment. I have spent the last 5 years working various levels in behavioral health, providing direct service to those struggling with co-occurring disorders.Using an eclectic and integrative approach, I incorporate the AIP model with EMDR, Person-in-Environment (PIE), Motivational Interviewing (MI), Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), family systems, interpersonal and solution-focused therapy along with Rogerian positive regard into my practice.