If you’re seeking rehab treatment for substance use addiction, understanding insurance coverage is often a barrier, as it’s complex. So let’s start with your rights.
Accessible addiction and mental health treatment is a right protected by the Mental Health Parity and Addiction Equity Act (MHPAEA). This law requires insurance plans that offer mental health and substance use disorder benefits to provide coverage that is comparable to medical/surgical coverage.
And The Affordable Care Act (ACA) classifies addiction and mental health treatment as one of the 10 essential health benefits. The ACA requires Marketplace, Medicaid expansion, Medicare, and most private plans to cover substance use disorder (SUD) services.
In this article, I clarify what Blue Cross Blue Shield (BCBS) typically covers for addiction rehab, explain the key factors that influence coverage, and provide a practical, step-by-step guide to verifying and using your benefits effectively.
Blue Cross Blue Shield Scope
As the nation’s largest health insurer, with the dominant market share in 40 states and the District of Columbia, Blue Cross Blue Shield (BCBS) contracts with about 90% of U.S. doctors and hospitals.
Its 34 independent companies collectively provide coverage for approximately 116 million Americans—about one in three people. This immense scale means understanding your BCBS benefits is a critical step for millions seeking addiction treatment.
Understanding the Levels of Care Covered by BCBS
BCBS generally covers rehab for substance use disorders, but the type of services, length of stay, and your out-of-pocket costs depend on your specific plan, state, and whether the provider is in-network.
Rehab is treated as an essential health benefit and must be covered comparably to medical/surgical care, subject to medical necessity review and benefit limits. BCBS plans generally follow the American Society of Addiction Medicine (ASAM) criteria, covering a continuum of care, as follows:
- Medical Detoxification
- Inpatient/Residential Rehab
- Partial Hospitalization (PHP)
- Intensive Outpatient (IOP)
- Outpatient Therapy
- Medication-Assisted Treatment (MAT)
- Dual-diagnosis care
Your cost share (deductible, copay, coinsurance) and any day/session limits are defined in your plan’s benefit summary.
Key Factors That Determine Your Specific Coverage
Several personal plan factors determine your out-of-pocket costs and available services.
- Plan Type and Metal Tier: Coverage varies by Blue company (e.g., Blue Cross NC, Medavie Blue Cross, BCBS state plans, FEP). HMO, PPO, EPO, and POS plans differ in network requirements and how Bronze, Silver, Gold, and Platinum tiers affect cost-sharing [1]
- Essential Health Benefits (EHB): Under the ACA, all ACA-compliant plans must cover mental and behavioral health services, including substance use disorder treatment.
Core Determinants
- Deductible, Copayments, and Coinsurance: It’s important to read your policy and understand the definitions and their financial impact.
- Out-of-Pocket Maximum: The critical financial protection cap.
- In-Network vs. Out-of-Network: In-network rehab programs usually have lower copays/coinsurance and easier authorization; some plans limit or exclude out-of-network care. There is a dramatic cost difference, and the importance of using in-network providers cannot be stressed enough.
- Medical necessity: Utilization management reviews documentation to confirm services are clinically necessary under your benefit plan.
- Preauthorization: Prior approval from BCBS, based on clinical assessment, is required for most inpatient and some outpatient services (residential, PHP, or IOP services). This is also called Verification of Benefits (VOB). Without authorization, you may have a denial or reduced payment.
- Visit or day limits: Some products limit the number of covered days or may require step-down through levels of care based on progress.
- Coverage for Families: Dependents are typically covered under family plans.
- Confidentiality: Seeking treatment is protected health information under HIPAA.
If Coverage Is Denied or Limited
Denials and restrictive authorizations are common, but there are structured ways to respond.
- Request a detailed explanation of benefits (EOB) showing the reason for denial (e.g., not medically necessary, no authorization, out-of-network).
- Ask for strong clinical documentation such as assessments, progress notes, and letters of medical necessity from physicians or therapists supporting the requested level of care.
- Follow your plan’s instructions and timelines to file an internal appeal. For urgent behavioral health needs, you can often request an expedited appeal.
- If you are eligible and the internal appeal is unsuccessful, pursue an external review via the process described in your policy documents.
Why Choose Northbound Treatment Services?
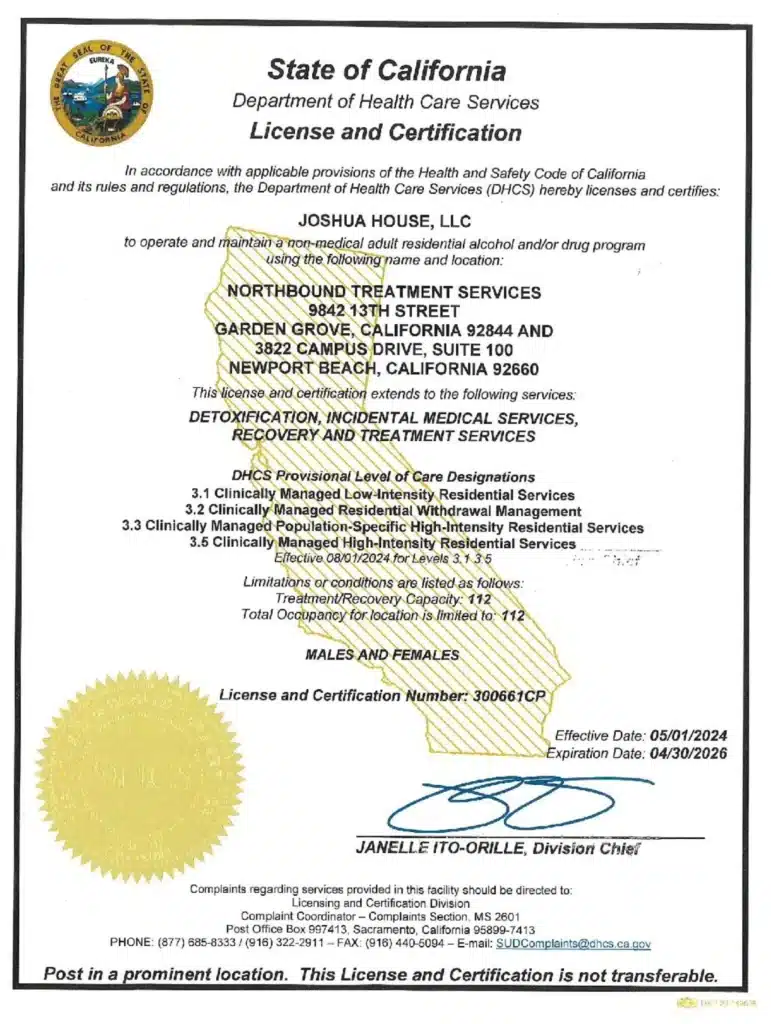
At Northbound, we have extensive experience helping patients overcome their substance abuse addictions, and we have a Christian faith-based track for those wishing to participate.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center for whatever time you may require.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment provides a flexible step-down from our residential program, allowing you to live at home and participate for several hours a day.
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] 2025 Blue Cross and Blue Shield Service Benefit Plan
Blue Cross Blue Shield. Find a Doctor.
Author
-

Chief Marketing Officer
Alexa Pelech is the Chief Marketing Officer at Northbound Treatment Services, where she combines her passion for helping others with a strong track record in addiction treatment marketing and outreach. Since joining Northbound in 2019, Alexa has held several key roles—including Referral Relations Manager and Director of Business Development—before stepping into her current leadership position in March 2023.Alexa began her career in behavioral healthcare as an Outreach Coordinator with American Addiction Centers, where she quickly developed a reputation for her compassionate approach and results-driven mindset. Today, she leads Northbound’s marketing strategy with the same energy and heart, driving growth while staying true to the mission of recovery.
Alexa holds a Bachelor of Arts in Fine and Studio Arts from San Francisco State University and later studied Substance Abuse and Addiction Counseling at Los Angeles Pierce College. Her creative background and commitment to service continue to shape her authentic, human-centered leadership style.