In the United States, the age-adjusted rate of drug overdose deaths jumped from 8.2 per 100,000 people in 2002 to 32.6 in 2022, largely due to opioid misuse [1]. That’s a 400% increase in twenty years!
Oxycodone and morphine are both opioids, but sometimes these drugs are called opiates. This can be confusing. Opioids is an umbrella term for all substances, natural or synthetic, that interact with opioid receptors in the brain. It is now the generally used term for this class of drugs [2].
Oxycodone is a semi-synthetic opioid derived from a substance in the poppy plant called thebaine. Opiates are naturally derived from the poppy plant and are a subset of opioids. Morphine is an opiate.
Both opiates and opioids may also be used illicitly by people with a substance use disorder.
Understanding Uses of Oxycodone and Morphine
Based on the structure of morphine, scientists have developed new drugs. Of the semi-synthetic opioids, heroin is made by acetylating morphine. Oxycodone and Hydrocodone are synthesized from thebaine, another compound found in the opium poppy.
Fully synthetic opioids are manufactured entirely in a laboratory and do not rely on a natural opiate base. Fentanyl is the most well-known and potent example; it is 50 to100 times more potent than morphine.
All these substances (whether natural morphine or synthetic fentanyl) work in the same fundamental way: they bind to opioid receptors (mu, kappa, delta) in the brain, spinal cord, and other parts of the body. This binding blocks pain signals and releases dopamine, creating feelings of pleasure and euphoria.
Both are used medically and may be prescribed for:
- Pain relief
- Anesthesia
- Cough suppression
- Diarrhea suppression
- Post-operative pain management
- Chronic pain management
- End-of-life care
- Treatment of opiate/opioid use disorder
Medical Uses and Effectiveness
The decision of which drug to use is made by medical doctors taking into consideration a number of factors.
For acute, severe pain in a hospital setting (IV route of administration): Morphine is often the first-line choice due to its rapid action, proven efficacy, and familiarity.
For chronic pain management (oral route of administration), oxycodone is frequently preferred because of its higher oral bioavailability, more predictable oral dosing, and potentially more favorable side effect profile (less itching, possibly less nausea).
For patients with kidney problems, oxycodone is often chosen over morphine due to a safer metabolite profile.
The following table summarizes some of their characteristics.
| Feature | Oxycodone | Morphine |
| Oral Bioavailability | Higher | Lower |
| Potency (oral) | Greater | Less |
| Typical uses | Moderate-to-Severe pain | Severe pain, cancer |
| Onset/Duration (oral) | Faster onset, longer (12h) | Slower onset, shorter duration |
| Abuse liability | Higher | Lower |
| Distinct side effects | More euphoria | More pruritus |
| Mechanism | Mu (some kappa) | Mu |
Oxycodone vs. Morphine: Side Effects and Addiction Potential
Both drugs share common opioid side effects due to their similar mechanism of action. However, key differences exist.
Shared common side effects include:
- Respiratory depression (slowed breathing) [3]
- Sedation
- Nausea
- Vomiting
- Constipation
- Dizziness
Main differences include:
- Morphine triggers a higher release of histamine. This can lead to more pronounced itching, flushing, and hypotension (low blood pressure).
- Oxycodone causes less histamine release, potentially resulting in less itching and hypotension. Some patients report differences in nausea or drowsiness, but this is highly individual.
Addiction Potential: Both oxycodone and morphine have a high and very similar potential for addiction and physical dependence due to their impact on brain reward pathways. They are both Schedule II controlled substances. The risk of addiction depends less on the specific drug and more on factors like dosage, duration of use, genetics, and personal history of substance abuse.
Potency: Oxycodone is about 1.5 times more potent than morphine when taken orally. This means a smaller milligram dose is needed for the same effect, which can sometimes be misperceived as making it “more addictive,” but the inherent abuse liability is comparable [4].
Onset and Formulations: Some formulations of oxycodone (particularly immediate-release) can have a slightly faster onset of action when taken orally. A rapid onset is often associated with a higher “rush” and greater reinforcing effects, which can contribute to abuse potential.
Signs of Prescription Drug Misuse
Oxycodone is commonly misused due to its availability in pill form, as it is widely prescribed, and easily diverted from its medical uses. Doctor shopping also is a major problem in which individuals obtain several prescriptions from different doctors, contributing to the opioid epidemic.
As with all addictive drugs, the high risk of escalating tolerance contributes to addiction. Withdrawal can be very intense, involving the following symptoms. Symptoms are often described as a severe, miserable flu and are highly variable in intensity. They are typically categorized into two phases:
Early Symptoms (Often beginning within 6-12 hours after the last dose for short-acting drugs like immediate-release oxycodone)
- Muscle aches and pain
- Anxiety, restlessness, and agitation
- Insomnia
- Runny nose, teary eyes
- Excessive sweating (diaphoresis)
- Yawning
Peak Symptoms (Usually within 1-3 days). 2-3 days for immediate-release oxycodone. Longer for extended-release oxycodone.
- Nausea, vomiting, and diarrhea
- Abdominal cramping
- Goosebumps and cold flashes (the origin of the term “cold turkey”)
- Dilated pupils
- Rapid heartbeat and high blood pressure
- Intense drug cravings
While acutely intense, the physical symptoms are not typically life-threatening for a healthy adult (unlike alcohol or benzodiazepine withdrawal). However, the severe discomfort and psychological cravings are a major reason for relapse. Some individuals may also experience a longer-term “post-acute withdrawal syndrome” (PAWS) with lingering anxiety, insomnia, and low energy.
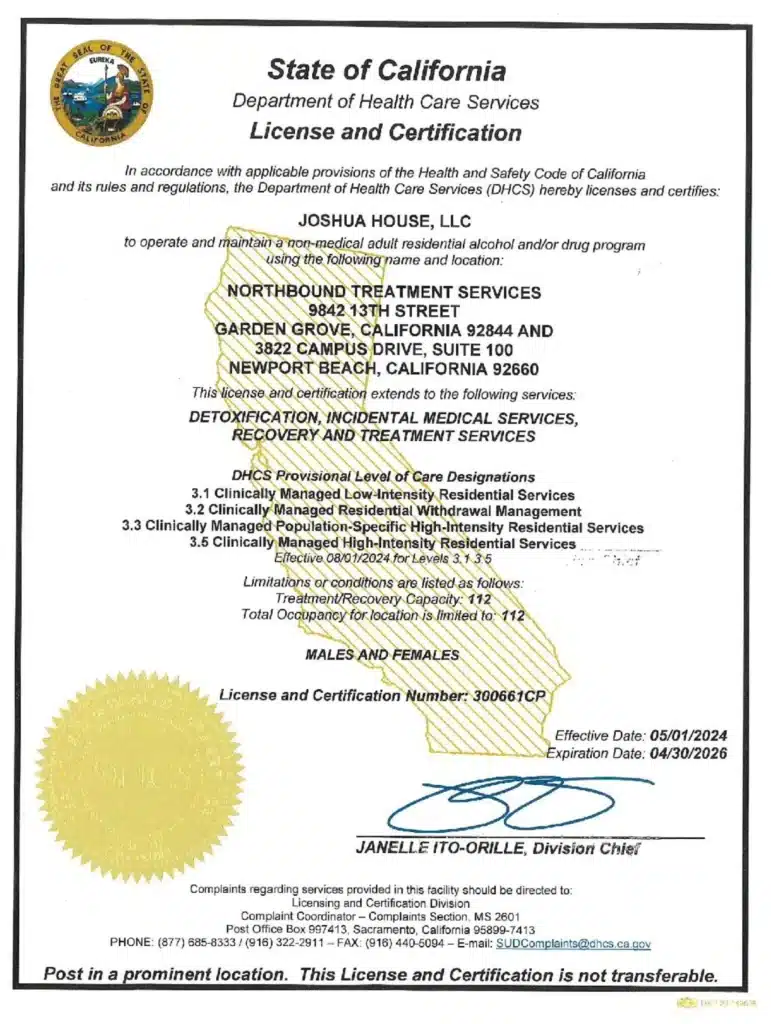
Treatment Options for Opioid Misuse at Northbound Treatment Services
At Northbound we offer medically supervised withdrawal management (detox) from opioids. A healthcare provider may create a tapering plan or use medications (like buprenorphine, clonidine, or others) to significantly reduce the severity of symptoms and ensure safety. Never stop taking prescription opioids abruptly without consulting your doctor.
We also offer residential treatment in our facilities in Orange County with individual, group and family therapy as appropriate, and outpatient programs.
When it’s Time to Seek Help, Point Your Compass Northbound
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Contact us!
Sources
[1] Spencer M. et al. 2024. Drug Overdose Deaths in the United States, 2002–2022. National Center for Health Statistics.
[2] Oregon Alcohol and Drug Commission. nd. Opiates or Opioids — What’s the difference?
[3] Mayo clinic. 2023. What are opioids and why are they dangerous?
[4] MD M.A.T.T. 2024. Morphine vs. Oxycodone: Differences, Similarities, Dosage.
Author
-

Clinical Director, Clinical Supervisor, EMDR Provider
I am a Licensed Clinical Social Worker and graduated with a degree from the USC School of Social Work in 2015 with an emphasis in mental health. I began my career working with the Orange County Welfare to Work Program providing mental health services to reduce barriers to employment. I have spent the last 5 years working various levels in behavioral health, providing direct service to those struggling with co-occurring disorders.Using an eclectic and integrative approach, I incorporate the AIP model with EMDR, Person-in-Environment (PIE), Motivational Interviewing (MI), Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), family systems, interpersonal and solution-focused therapy along with Rogerian positive regard into my practice.