Gabapentin is a versatile, FDA-approved prescription medication used to treat many conditions. At the federal level, it is not considered a narcotic, but a number of states consider it a controlled substance due to potential for abuse. Read on to learn more about what it is used for, risks, and side effects.
What is Gabapentin?
Gabapentin is a versatile anticonvulsant (anti-seizure) medication. Its chemical structure is similar to a brain chemical called gamma aminobutyric acid (GABA) which calms excited neurons. GABA reduces the excitability of neurons in the brain, which play a role in seizures and the transmission of pain signals.
As such, gabapentin was primarily intended to treat epileptic seizures and nerve pain that occurs after shingles. The exact way it works isn’t fully understood but it is believed to affect the activity of calcium channels in the brain and nervous system, helping to calm overactive nerves. However, interestingly, it doesn’t actually bind to GABA receptors [1].
Gabapentin is also used for “off-label” treatment of other conditions. One report in 2022 said it was among the ten most prescribed medications in the US.
What is Gabapentin Prescribed For?
Gabapentin is FDA-approved for:
- Helping to control convulsions (partial seizures) in epilepsy.
- Neuropathic pain that occurs after shingles and in diabetes.
- Restless Legs Syndrome with a variant called gabapentin enacarbil.
Up to 95% of gabapentin use today is prescribed for off-label (not FDA approved) indications including, but not limited to:
- As an alternative to opioid therapy for pain management
- Restless Legs Syndrome
- Periodic Limb Movement Disorder (PLMD)
- Hot flashes and night sweats in post-menopausal women and those undergoing cancer treatment
- Migraine prevention
- Fibromyalgia
- Alcohol and drug withdrawal symptoms
- Anxiety disorders
- Bipolar Disorder
- Obsessive Compulsive Disorder (OCD)
Risks and Side Effects of Gabapentin
Gabapentin should only be taken under the supervision of your doctor and exactly as prescribed.
As with most medications, there are side effects and risks. Gabapentin should not be taken if you are taking Isocarboxazid. There is a long list of possible medications which gabapentin may interact with but this requires discussion with your doctor.
Gabapentin can interact dangerously with:
- Opioids (e.g., hydrocodone, oxycodone)
- Alcohol and other CNS Depressants (e.g., benzos, sleeping pills)
- Antacids
There are many possible side effects which must be discussed with your doctor. The most common ones include [2]:
- Signs of an allergic reaction
- Changes in mood or behavior
- Signs of kidney abnormalities
- Other concerning abnormalities: Change in color of your skin to a bluish color on your lips, nail beds, fingers, or toes along with severe fatigue or weakness and unexpected muscle pain.
- Cold or flu-like symptoms
- Delusions
- Dementia
- Hoarseness
- Lack or loss of strength
- Lower back or side pain
- Swelling of the hands, feet, or lower legs
Regulations and Misuse Potential
In 1993, the FDA approved Neurontin, the original branded gabapentin, for helping to control partial seizures. The manufacturer engaged in widespread marketing campaigns to promote the drug for off-label use to control pain.
However, without controlled studies across a range of types of pain, the FDA did not grant approval for this indication. To this day, there are limited adequate controlled studies on the efficacy of off-label uses of gabapentin, despite its widespread use.
One study of off-label clinical trial research revealed insufficient controlled trial evidence to demonstrate the efficacy of gabapentin for [3]:
- Depression
- Bipolar Disorder (despite marketing efforts to promote this indication)
- Alcohol
- Cocaine
The study concluded “most of the evidence for off-label use is limited to a few small, low-quality studies, often with data only weakly supporting use. Given this, and its potential for misuse and dependence, gabapentin should be taken with this knowledge and only as prescribed”.
Recently there has been an alarming increase in reports of recreational gabapentin abuse or intentional misuse among those with known substance use disorders (SUDs) and consequent harm. The rate of gabapentin abuse among patients with known substance use disorders was found to be notably higher, in the range of 15% to 22%.
Gabapentin can enhance the psychological effect of opioids by producing feelings of relaxation, calmness, and euphoria, especially at high doses. It is sometimes misused to potentiate the effects of opioids, benzodiazepines, and marijuana and has contributed to drug overdose deaths. As a result, the risk profile of gabapentin may be higher than previously thought [3].
Recent guidelines from the Centers for Disease Control and Prevention (CDC) recommend that other medication classes be considered before beginning opioids for chronic noncancer pain, which includes a recommendation of gabapentin as a first-line agent for neuropathic pain.
Due to the growing misuse of gabapentin, many states have tightened regulations around it, driven by several factors:
- Potential for Abuse and Misuse: It is sometimes combined with opioids, benzodiazepines, and marijuana to potentiate the effects.
- Overdose Risk: When combined with other CNS depressants like opioids, it significantly increases the risk of life-threatening respiratory depression.
- Withdrawal Symptoms: For those taking high doses for prolonged periods.
- Epidemiological Data: States hit hardest by the opioid crisis (like Kentucky, West Virginia, and Tennessee) were among the first to schedule gabapentin, based on overdose death reports showing gabapentin. Many others have followed.
These new regulations now involve:
- Stricter rules for prescriptions.
- Pharmacists must report your prescription to the state database.
- Doctors must check the Prescription Drug Monitoring Program (PDMP) before prescribing it to you, to see your history of other controlled medications.
- Transferring prescriptions between pharmacies may be more difficult.
- Traveling with the medication across state lines can become complicated, as its legal status changes.
Comprehensive Dual Diagnosis Treatment At Northbound
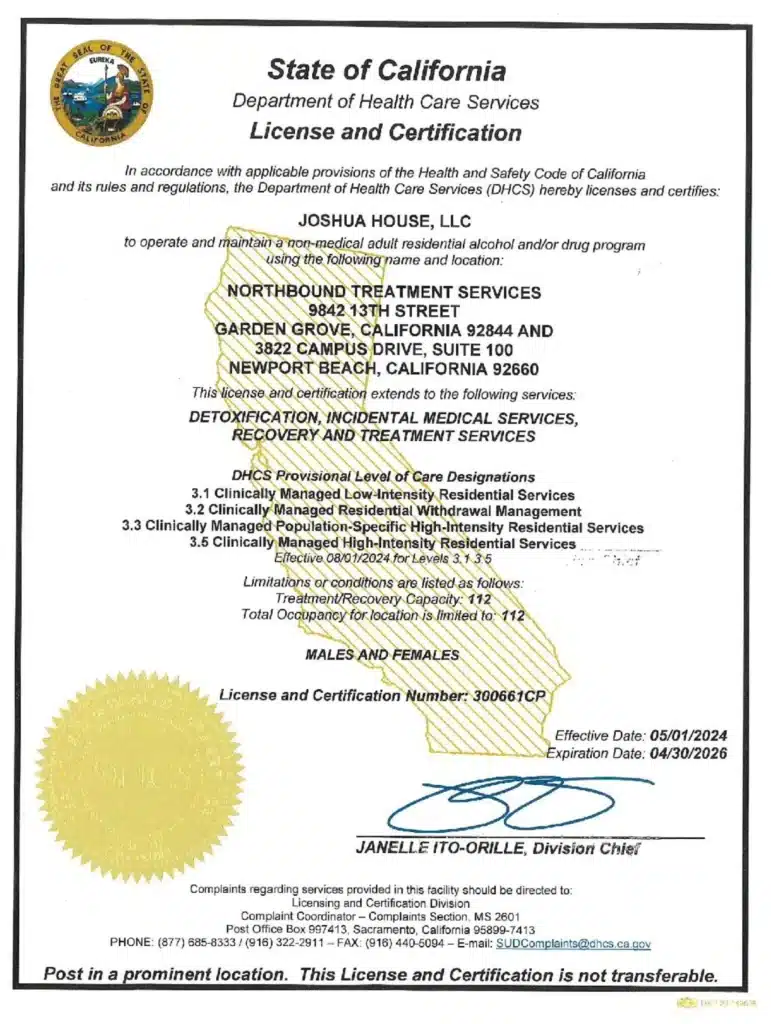
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] Catanese, L. 2024. Gabapentin: Uses, side effects, and what you should know if you’ve been prescribed this medication. Harvard Health.
[2] Mayo Clinic. Gabapentin (oral route).
[3] Peckham, A. M., Evoy, K. E., Ochs, L., & Covvey, J. R. (2018). Gabapentin for Off-Label Use: Evidence-Based or Cause for Concern?. Substance abuse : research and treatment, 12.
Author
-

Clinical Director, Clinical Supervisor, EMDR Provider
I am a Licensed Clinical Social Worker and graduated with a degree from the USC School of Social Work in 2015 with an emphasis in mental health. I began my career working with the Orange County Welfare to Work Program providing mental health services to reduce barriers to employment. I have spent the last 5 years working various levels in behavioral health, providing direct service to those struggling with co-occurring disorders.Using an eclectic and integrative approach, I incorporate the AIP model with EMDR, Person-in-Environment (PIE), Motivational Interviewing (MI), Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), family systems, interpersonal and solution-focused therapy along with Rogerian positive regard into my practice.