Bipolar Disorder, formerly called manic-depressive illness, is a brain disorder that causes unusual shifts in a person’s mood, energy, and ability to function. It is one of the top 10 leading causes of disability worldwide [1].
It affects 2.8% of the adult population in the US. Of that group, slightly more men (2.9%) are affected than women (2.8%) [3].
In this article, I look at Bipolar Disorder symptoms, bipolar disorder in men, and the special challenges they face, and treatment options.
Key Facts About Bipolar Disorder
Bipolar Disorder (BD) is characterized by chronically occurring episodes of mania or hypomania alternating with depression. There are two peaks in the age of onset: 15-24 years and 45-54 years, with more than 70% showing symptoms before 25 years of age. In adulthood, more than 60% of patients with BD report at least one “stressful life event” before a manic or depressive episode in the preceding 6 months [1].
Bipolar disorder is a very serious mental health condition. Of those diagnosed with BD [4]:
- One-third will attempt suicide in their lifetime
- 16% will have attempted suicide within the past year
- 6% to 7% complete suicide
Symptoms of Bipolar Disorder
Bipolar Disorder is not just “being moody”. It is complex to diagnose as there are a number of overlapping symptoms from other mental health conditions. Most patients with BD are not correctly diagnosed until approximately 6 to 10 years after first contact with a healthcare provider, despite the presence of clinical characteristics of the condition [1].
There are several types of Bipolar Disorder. For simplicity, I will focus on the two most common. Here is an outline of symptoms:
Bipolar Disorder I
At least one manic episode, which might have been preceded or followed by a hypomanic episode or major depressive episode (hypomanic or major depressive episodes are not required for the diagnosis).
Manic episode: A distinct period of abnormally and persistently elevated, expansive, or irritable mood and increased activity or energy, lasting at least 1 week (or any duration if hospitalization is necessary).
Hypomanic episode: A distinct period of abnormally and persistently elevated, expansive, or irritable mood and increased activity or energy, lasting at least 4 consecutive days.
Major Depressive Episode (MDE): A period of at least 2 weeks of depressed mood or loss of interest/pleasure, with 5 or more specific symptoms daily or nearly every day.
The following BD symptoms are those required by the DSM-5, the manual psychiatrists use to diagnose mental health conditions [N].
| BD-1 DSM-5 Diagnostic CriteriaThree or more of the following symptoms (four if the mood is only irritable) must be present to a significant degree and represent a noticeable change from usual behavior: | ||
| Inflated self-esteem or grandiosity | Decreased need for sleep (e.g., feeling rested after only 3 hours) | More talkative than usual or pressure to keep talking |
| Flight of ideas or subjective experience that thoughts are racing | Distractibility | Increase in goal-directed activity (socially, at work/school, or sexually) or psychomotor agitation |
| Excessive involvement in activities that have a high potential for painful consequences (e.g., unrestrained buying sprees, sexual indiscretions, foolish business investments) | ||
| Other Symptoms | ||
| Excessively “high,” overly good, euphoric mood | Unrealistic beliefs in one’s abilities and powers | Extreme irritability |
| A lasting period of behavior that is different from usual | Provocative, intrusive, or aggressive behavior | Abuse of drugs, particularly cocaine, alcohol, and sleeping medications |
| Increased sexual drive | Poor judgment | Denial that anything is wrong |
Bipolar Disorder II
At least one current or past hypomanic episode and a major depressive episode; never a manic episode.
| BD-II DSM-5 Diagnostic CriteriaFive or more of the following symptoms must be present to a significant degree and represent a noticeable change in functioning. | ||
| Depressed mood most of the day, nearly every day | Markedly diminished interest or pleasure in all, or almost all, activities | Significant weight loss or change in appetite |
| Insomnia or hypersomnia | Psychomotor agitation or retardation | Fatigue or loss of energy |
| Feelings of worthlessness or excessive guilt | Diminished ability to think or concentrate | Recurrent thoughts of death or suicide |
| Other Symptoms | ||
| Feelings of sadness that don’t go away | Increased risk-taking behavior, including reckless driving or substance abuse | Chronic pain or other physical problems that don’t respond to treatment |
| Irritability or restlessness | Repeated thoughts of death or suicide | |
Men and Bipolar Disorder: Out of the Shadows
The fact that it takes 6 to 10 years for a BD diagnosis to be made after first contact with a healthcare provider presents unique challenges for men. In fact, men suffering from bipolar are less easy to identify and less likely to seek assistance and treatment than women. But, when men experience symptoms, they tend to be more severe than in women.
Men Struggle with Stigma Around Bipolar Disorder
Men still living with stigma around mental health may not be comfortable referring to themselves as a person with a mental health condition. They may shy away from seeking help and opening up about their emotions and feelings due to concerns of weakness.
In a culture where traditional masculine values of stoicism and resilience prevail, and where usually it is depression, not mania, that causes an individual to see a medical professional, men are less likely to recognize the disorder in themselves for fear of being judged as weak.
So denial is common. And men may be more inclined to deny the problem, since it deals with emotional extremes and men are taught not to show emotion, nor be depressed [3].
Challenges in Diagnosing and Living With Bipolar Disorder in Men
On the contrary, mania, with its elevated mood, grandiose sense of well-being, and overconfidence, can be harder to detect in men, where confidence is associated with masculinity. Men are more likely to experience more frequent and severe symptoms of manic episodes, often with aggressive behaviors.
This makes it harder to identify atypical behaviors in men, delaying diagnosis and treatment at great cost to the man and their loved ones coping with them.
Similarly, the poor decision-making, risk-taking, or reckless behaviors may be masked under the guise of self-confidence, again delaying seeking medical help.
With the depressive side of the illness, BD carries a high risk of suicide. And men have a much higher rate of attempts and completed suicide rates in comparison with women.
Whereas women tend to seek help for depression, many men remain in denial, making excuses for their behavior as being “just down in the dumps” or “just irritable”, as depression flies in the face of male norms of independence and emotional control.
But depression also is very visible to loved ones and friends. The challenge is helping men accept that and seek help before it’s too late. Another challenge is that there is little awareness, resources, conversations, and support specifically for men about men’s mental health and bipolar disorder.
Providing Support to Men With Bipolar Disorder
It can be difficult to raise with a man the delicate topic of the need to seek help. Here are some suggestions:
- Find a convenient time where there is room to explore the topic without rushing
- Find a comfortable space for both of you to talk.
- Express your concern and your care for him.
- Try to maintain your composure so as not to overwhelm him with your feelings, as justified as they may be.
- Don’t point out his behaviors that upset you. Avoid criticism and antagonizing him.
- Share that something out of your and his control may be a factor for the concerning behaviors.
- Reinforce that most mental health conditions are treatable. Support him by saying you offer to help him get the help he needs and that he’s not alone.
Treatment Options for Bipolar Disorder
BD is treatable, but early diagnosis is critical. Mania is considered a medical emergency, warranting emergency department visits if no other help is available.
Medications
Medications are the mainstay of therapy and are selected depending on the phase of illness, severity, and patient factors such as prior responses or current medications. A full medical diagnosis by a psychiatrist is necessary to determine the best course of treatment. Each form of BD requires different medications. The following are FDA-approved [4]. There are others.
- Lithium salts: The “gold standard”.
- Atypical antipsychotics (e.g., Abilify, Latuda, Olanzapine, Quetiapine)
- Anticonvulsants (e.g., Valproic acid, Lamotrigine)
Therapy
Stress is known to trigger manic and depressive symptoms. Behavioral interventions, including basic psychoeducation and Cognitive Behavioral Therapy, among others, are evidence-based supports to medications that improve social function and reduce the need for medications, number of hospitalizations, and relapse rates.
In addition, nutrition, exercise, coping strategies, and positive attitudes toward good health are beneficial.
There is hope. BD is treatable and symptoms can be managed. And there is strength in summoning the courage to seek help.
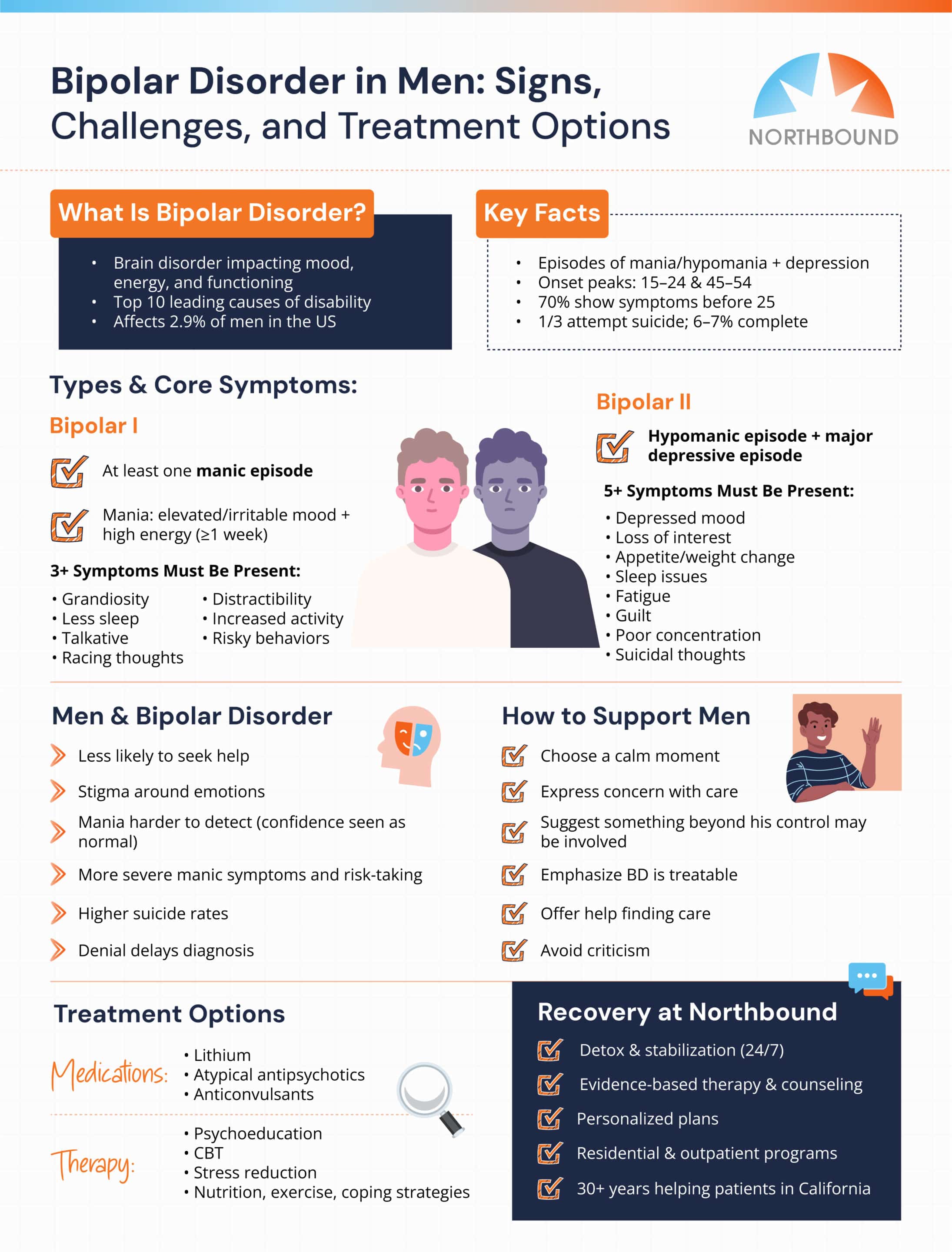
Seeking Help and the Path to Recovery at Northbound
At Northbound, we have extensive experience helping patients overcome their substance abuse addictions, and with a faith-based track for those wishing to participate.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center for whatever time you may require.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment provides a flexible step-down from our residential program, allowing you to live at home and participate for several hours a day.
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] Jain A, Mitra P. Bipolar Disorder. [Updated 2023 Feb 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-.
[2] International Bipolar Foundation. Bipolar Disorder in Men.
[3] Montero, H. 2022. Bipolar Symptoms in Men: 10 Signs to Look For Healthcentral.com
[4] Marzani G and A. Price Neff. 2021. Bipolar Disorders: Evaluation and Treatment. Am Fam Physician. 2021;103(4):227-239.
[5] American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed., text rev.).
Author
-

Program Director
Amanda has been working in the behavioral healthcare field since 2011. During her career, she worked her way through various positions in behavioral healthcare and finally earned a position as a program director over 10 years ago. Amanda initially graduated with her license in vocational nursing and an associate degree with completed certifications in substance use and abuse. Amanda has continued on in her education, and she obtained her bachelor’s degree in the science of nursing obtaining a BSN, and her RN licensure. With a primary background in nursing and medical care, and a proven track record in leadership positions in Behavioral Healthcare, Amanda is the perfect person to manage the daily medical and clinical services of a healthcare treatment facility.
As the Executive Director of Northbound, she utilizes her personal recovery experience coupled with her professional experience to oversee the clinical, medical, and the overall operational function of the organization. She believes that above all else the quality of client care should be the top priority for all the employees at Northbound. She pushes clients to find passion in recovery and to gain meaningful and impactful messages in the group programming to provide lasting recovery.
Amanda has a 17-year-old son. She has a passion for fitness and enjoys Rock Climbing and backpacking in her free time. Her passion for the outdoors plays a major role in her content creation in the daily programming for the schedule at Northbound.