Seeking help for addiction takes courage. For those insured by Cigna, understanding insurance coverage from Cigna can be confusing. Knowing your options is a big step to obtaining affordable treatment.
When medically necessary, Cigna plans cover rehab, but access and costs depend heavily on your specific policy, network status, and precertification (prior authorization).
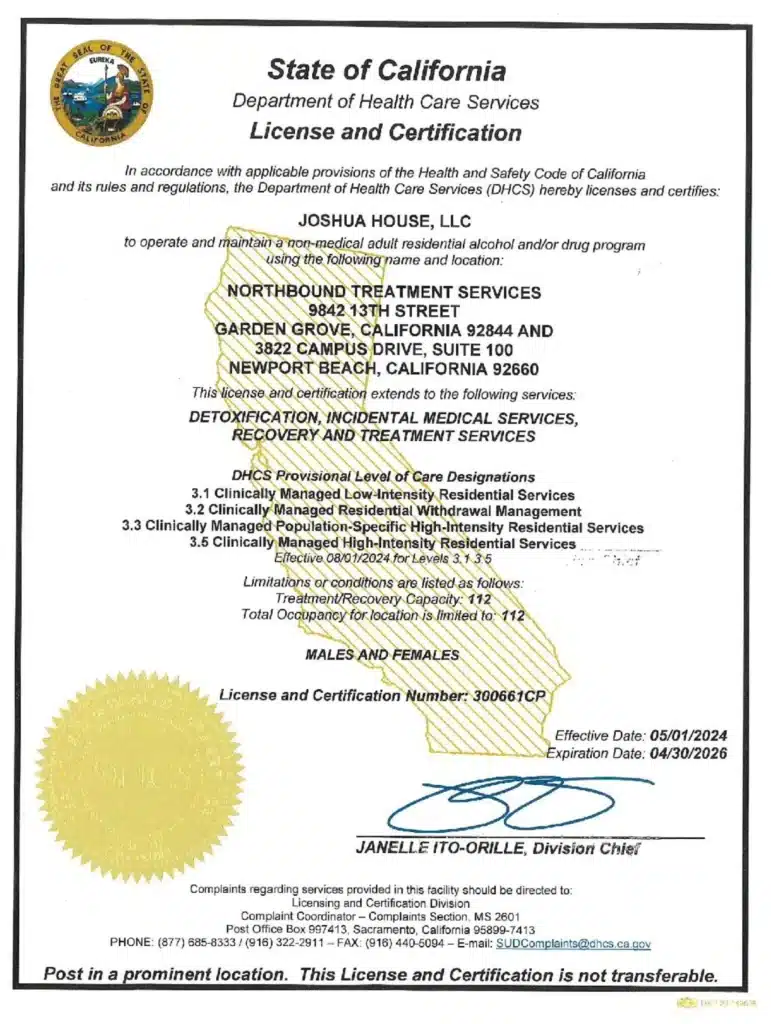
Verify your benefits with Cigna and the help of the admissions team at a rehab that is in-network with Cigna, such as Northbound Treatment Services. Then complete any required preauthorization before admission.
This article provides a step-by-step overview of Cigna’s addiction treatment coverage and how to access your benefits.
Understanding Cigna’s Coverage for Addiction Treatment
Cigna covers addiction treatment as mandated by the Mental Health Parity and Addiction Equity Act. It requires insurers like Cigna to cover behavioral health services at a level comparable to medical or surgical care.
Cigna usually covers this continuum of care [1]:
- Medical Detoxification: Medically supervised withdrawal management for alcohol and drugs when medically necessary.
- Inpatient/Residential Rehab: 24/7 live-in treatment. Often, this is done with an initial short authorization window that can be extended based on clinical documentation.
- Partial Hospitalization (PHP): Day programs with medical support.
- Intensive Outpatient (IOP): Several hours of therapy, multiple days a week.
- Standard Outpatient & Aftercare: Ongoing therapy and support groups with standard outpatient counseling and aftercare.
- Medication‑assisted treatment (MAT): For opioid and alcohol use disorders (for example, buprenorphine or naltrexone) alongside therapy.
Step‑by‑Step: Using Cigna for Rehab
Gather Your Information
Clarify Clinical Need
- Get a brief assessment from a physician, therapist, or an admissions clinician to document diagnosis, substances, use pattern, and risk level.
- Higher‑risk presentations (e.g., severe withdrawal risk, suicidality, lack of safe housing) support medical necessity for detox or inpatient/residential levels of care.
Contact Cigna with 9 Key Questions
- Call: Use the member services number on the back of your card.
- What to Ask: Here are 9 key questions:
- “Do I need a pre-authorization or referral to enter treatment?”
- “What is my deductible, copay, or coinsurance for in-network vs. out-of-network rehab?”
- “What levels of care are covered (detox, residential, PHP, IOP, outpatient, MAT)?”
- “What is In‑network vs out‑of‑network coverage and any exclusions?”
- “Can you provide a list of in-network addiction treatment facilities near me or for the level of care I need?”
- “What are the deductibles, copays, and coinsurance for in‑network SUD services?”
- “Are there any visit or day limits?”
- “Are extensions allowed based on medical necessity?”
Use Cigna’s Digital Tools
Go to the Cigna website and mobile app to search for in-network providers using their “Find a Doctor” tool (filter for “Behavioral Health” or “Substance Use Treatment”).
Contact Potential Rehabs Directly
- Once you have a shortlist, call the facility directly. Use Cigna’s online provider directory or ask the Cigna representative for in‑network SUD facilities (detox, residential, PHP/IOP).
- The facilities’ admissions teams have daily experience verifying Cigna benefits. They can often check your coverage quickly and give you a clear picture of expected costs, program openings, and the admissions process.
- Many programs’ websites list Cigna as an accepted insurer and offer instant “insurance verification” forms that allow their admissions team to check your benefits directly.
- If the clinically appropriate program is out‑of‑network, ask about a single‑case agreement or in‑network exception when no comparable in‑network option is reasonably available.
Complete Precertification (Preauthorization)
- Many Cigna plans require prior authorization for inpatient and, often, for PHP. Outpatient and IOP may or may not need it [4].
- The treating facility usually submits clinical information (diagnosis, American Society of Addiction Medicine (ASAM) level of care, risk factors) to obtain an initial approval window (for example, several days of detox or a short residential stay).
- Ongoing days are then authorized based on continued‑stay reviews documenting progress and persisting clinical need.
During and After Treatment
- Track explanations of benefits (EOBs) to confirm claims are processed at the expected in‑network rate and to catch any denials early.
- Work with case management, if offered, for step‑down planning to PHP/IOP, outpatient therapy, MAT, and peer recovery supports, which Cigna commonly covers as continuing care.
Cost and Plan Type Considerations
Plan type (HMO, PPO, EPO, employer vs marketplace) strongly influences network rules and cost‑sharing.
Bronze‑tier marketplace plans often have lower premiums but higher deductibles; inpatient SUD care may be covered at 0% coinsurance only after the deductible is met.
Silver/Gold tier plans may have lower coinsurance for in‑network rehab, but still require preauthorization and adherence to network rules.
What If My Claim is Denied or I Can’t Find a Bed?
Initial denials or network issues can happen. You can appeal with support from your treatment provider. Contact the rehab’s admissions team for help, as they often have experience with appeals. Cigna also has case management or patient advocacy services which you could use as a resource.
You don’t have to figure it out alone. Start today by making that first call to Cigna or directly to a treatment center that can guide you. Recovery is possible, and your insurance is an important tool to help you access it.
Why Choose Northbound Treatment Services?
At Northbound, we have extensive experience helping patients overcome their substance abuse addictions, and with a Christian faith-based track for those wishing to participate.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center for whatever time you may require.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment provides a flexible step-down from our residential program, allowing you to live at home and participate for several hours a day.
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] Cigna Healthcare. Inpatient and Outpatient Treatment for Substance Use Disorder.
[2] Cigna Healthcare. Types of Health Insurance.
[3] Cigna Healthcare. Claims and Explanation of Benefits (EOB).
[4] Cigna Healthcare. Precertifications.
Author
-

Clinical Director, Clinical Supervisor, EMDR Provider
I am a Licensed Clinical Social Worker and graduated with a degree from the USC School of Social Work in 2015 with an emphasis in mental health. I began my career working with the Orange County Welfare to Work Program providing mental health services to reduce barriers to employment. I have spent the last 5 years working various levels in behavioral health, providing direct service to those struggling with co-occurring disorders.Using an eclectic and integrative approach, I incorporate the AIP model with EMDR, Person-in-Environment (PIE), Motivational Interviewing (MI), Cognitive Behavioral Therapy (CBT), Dialectical Behavioral Therapy (DBT), family systems, interpersonal and solution-focused therapy along with Rogerian positive regard into my practice.