Seeking help with rehab for substance abuse is a courageous step. But if you are an Aetna policyholder, you may be wondering what coverage Aetna provides for this? Aetna is one of the largest health insurance providers in the U.S., covering over 22.1 million people in its ~22.1 million Commercial and Government health insurance plans (Medical).
Aetna does cover rehab for substance abuse and related mental health conditions with comprehensive benefits, a strong provider network, and additional mental health resources. They offer personalized treatment recommendations based on medical necessity.
What this coverage depends on is what services are covered, the length of treatment, your specific plan, medical necessity, and requirements for prior authorization. In this article, I explain how coverage works and the steps to get started.
What Aetna Covers
Federal law governs this coverage. Under the Affordable Care Act (ACA), Aetna must cover essential health benefits, similar to other medical benefits, including:
- Mental health and substance use disorder services
- Behavioral health treatment (including psychotherapy and counseling)
So this is a mandated benefit, but the specific level of coverage is dictated by your individual plan (e.g., HMO, PPO, Medicare Advantage) [1]. It’s very important to stay in-network to minimize costs. In-network plans can provide a 0% coinsurance, while out-of-network options may vary and could require pre-certification. Treatment cannot begin without it in most cases.
Aetna maintains a network of preferred rehab facilities. They must pass a thorough screening for quality care and adherence to modern treatment principles. Using an in-network provider means higher coverage levels. This can lead to reduced out-of-pocket expenses for individuals seeking treatment.
Aetna offers potential coverage for out-of-network rehab services, but the breadth of coverage is generally lower compared to in-network services, often leading to higher out-of-pocket expenses for the insured. Out-of-network rehab programs typically come with increased costs compared to in-network services. Out-of-network providers have not been subjected to the same quality screening as in-network programs.
What Types of Rehab Does Aetna Cover?
Aetna covers a continuum of care from intensive to outpatient support, as follows:
- Medical Withdrawal Management (Detox): In an inpatient or hospital setting, this is frequently covered as a medically necessary first step. In-network providers have the best rates.
- Inpatient/Residential Rehab: When symptoms or withdrawal cannot be safely managed at a lower level of care, coverage is provided for stabilization and intensive treatment. Pre-authorization is almost always required. Length of stay is based on medical necessity.
- Partial Hospitalization Programs (PHP): This is a day treatment model. It is often covered as a step-down from inpatient or an alternative to it for moderate-severity cases.
- Intensive Outpatient Programs (IOP): This provides several hours per week and is typically well covered.
- Standard Outpatient Therapy and Aftercare: Regular counseling and support groups, typically for relapse prevention, are usually covered with a standard co-pay. Aetna’s ongoing support services are crucial for individuals transitioning back into daily life after treatment. These services aim to maintain connections to care and provide resources that support sustained recovery.
- Medication-assisted Treatment: For opioid (buprenorphine and methadone programs) or alcohol use (naltrexone) disorders, when medically necessary.
- Co-occurring mental health treatment, such as for depression, anxiety, PTSD, etc., when delivered in a behavioral health setting.
Medical Necessity and Levels of Care
To determine which level of care it will authorize, Aettna uses medical necessity criteria such as those from the American Society of Addiction Medicine (ASAM) or similar guidelines. Usually, the treatment provider will handle this step.
When withdrawal is moderate to severe or unsafe to manage in an outpatient setting due to risk of seizures, delirium tremens, unstable vital signs, or complex polysubstance abuse, inpatient withdrawal management is generally approved.
When 24-hour monitoring is needed due to high relapse risk, unsafe home environment, severe functional impairment, or recent failed lower levels of care, residential or inpatient rehab is usually authorized.
When the person can safely live at home but still needs structured therapy several days a week,
Lower-intensity options such as PHP, IOP, or standard outpatient care are used.
Prior Authorization or Precertification
“Precertification” (prior authorization) for higher levels of behavioral health care is commonly required by Aetna. This is generally a non-negotiable, critical step. Typically, this includes:
- All inpatient admissions for withdrawal management or rehab
- Residential treatment center (RTC) stays
- Partial hospitalization programs (PHP)
- Some specialized services
Treatment providers usually initiate precertification by phone, fax, or online through Aetna/Availity, the provider portal. If Aetna is notified within a set timeframe (often 24-48 hours), emergency admissions can be authorized retroactively. It’s common to have continued stay reviews. Aetna may approve a set number of days (e.g., 5-7 inpatient days) and then require clinical updates to extend coverage.
Costs: Deductibles, Copays, and Limits
Your out-of-pocket costs depend on plan type (e.g., HMO vs PPO, Bronze or Gold), network status, and whether deductibles have been met. Typical cost-sharing structures may include:
- A deductible you must pay before Aetna pays a percentage of rehab costs.
- Coinsurance (e.g. 20-40% of the allowed charge) for inpatient or PHP/IOP services after the deductibles.
- Fixed copays for outpatient therapy visits, which may be low or zero in better plans.
- Out-of-pocket maximum: Once this is met, Aetna covers 100% of in-network care.
Many plans cap the number of covered behavioral health visits (e.g., a set number of rehab or therapy visits per year), though federal parity rules require that these limits be comparable to medical/surgical benefits.
How to Check Your Specific Aetna Plan
The safest approach is to confirm exact rehab coverage directly as benefits vary by state, employer, and metal tier (Bronze or Gold).
- Call the number on the back of the Aetna ID card. Ask about “substance use disorder treatment benefits” for inpatient, residential, PHP, IOP, MAT and outpatient therapy.
- Ask if your preferred facility is in-network and whether precertification is required for the planned level of care.
- Ask for information on deductibles, copays/coinsurance, visit or day limits, and any prior-authorization rules for detox, residential, and MAT.
Alternatively, contact the rehab facility’s admissions team. They have experience verifying benefits and navigating pre-authorization with Aetna. They will help you.
Aetna has a network of approved addiction treatment providers, but not all rehab facilities accept Aetna insurance.
Factors That Affect Coverage:
- In-Network vs. Out-of-Network: In-network providers typically cost less, while out-of-network providers may result in higher out-of-pocket expenses.
- Treatment Type: Some Aetna plans may offer more comprehensive coverage for inpatient rehab than outpatient treatment.
- Location: Coverage policies vary by state and facility
What to Do If You Face a Denial or Challenge
Initial denials or requests for more information are not uncommon and are part of the process.
The appeals process is a right. The rehab facility can often assist with appeals and peer-to-peer reviews.
Seeking Help and the Path to Recovery at Northbound
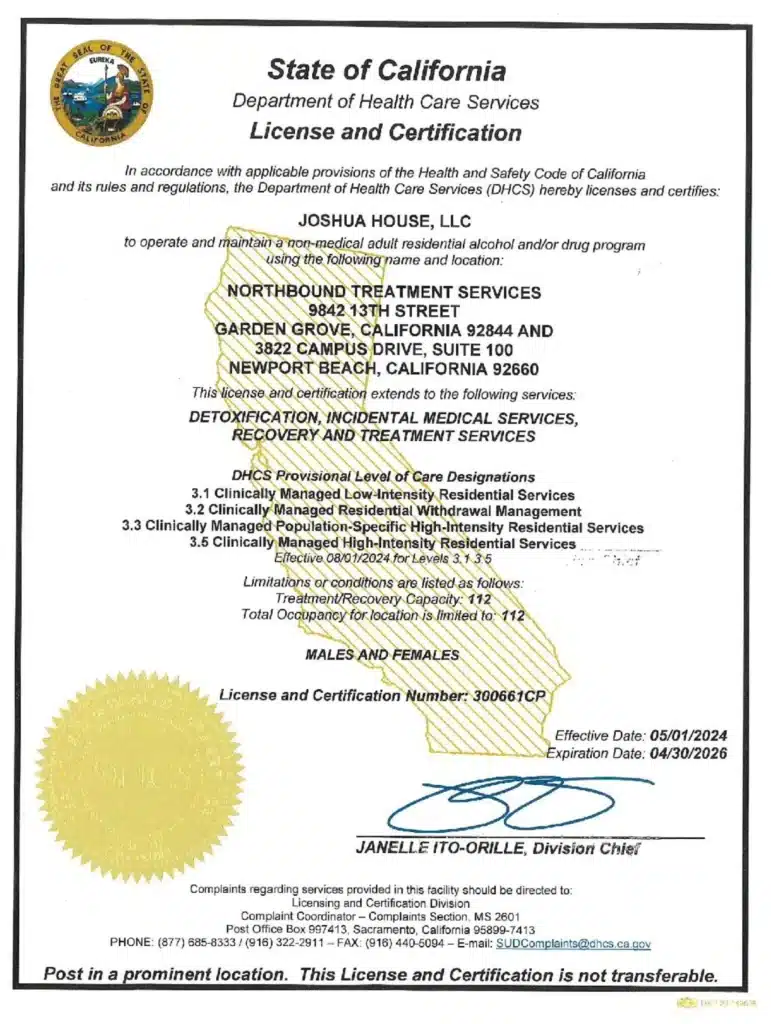
At Northbound, we have extensive experience helping patients overcome their substance abuse addictions, and with a Christian faith-based track for those wishing to participate.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center for whatever time you may require.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment provides a flexible step-down from our residential program, allowing you to live at home and participate for several hours a day.
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] Aetna. HMO, PPO, POS, EPO, & HDHP: What’s the Difference?
[2] Aetna. Find a doctor, dentist or hospital.
Aetna. Summary of Benefits and Coverage: 2025 TX Gold 4 Advanced HMO AI/AN CSR LTD.
Author
-

Program Director
Amanda has been working in the behavioral healthcare field since 2011. During her career, she worked her way through various positions in behavioral healthcare and finally earned a position as a program director over 10 years ago. Amanda initially graduated with her license in vocational nursing and an associate degree with completed certifications in substance use and abuse. Amanda has continued on in her education, and she obtained her bachelor’s degree in the science of nursing obtaining a BSN, and her RN licensure. With a primary background in nursing and medical care, and a proven track record in leadership positions in Behavioral Healthcare, Amanda is the perfect person to manage the daily medical and clinical services of a healthcare treatment facility.
As the Executive Director of Northbound, she utilizes her personal recovery experience coupled with her professional experience to oversee the clinical, medical, and the overall operational function of the organization. She believes that above all else the quality of client care should be the top priority for all the employees at Northbound. She pushes clients to find passion in recovery and to gain meaningful and impactful messages in the group programming to provide lasting recovery.
Amanda has a 17-year-old son. She has a passion for fitness and enjoys Rock Climbing and backpacking in her free time. Her passion for the outdoors plays a major role in her content creation in the daily programming for the schedule at Northbound.