It takes courage to seek help for addiction or mental health conditions. The first questions most people ask are, “What is the cost, and what is covered?
Yes, insurance typically covers rehab in some form. This is due to major legal and policy shifts in the last fifteen years, with federal laws like the Affordable Care Act (ACA) and the Mental Health Parity and Addiction Equity Act (MHPAEA). They mandate coverage as an essential health benefit on par with medical care.
Nonetheless, coverage is not a simple “yes/no”, as it depends on your plan, your state, the type of rehab, and specific criteria. Insurance coverage for rehab is complex. It can present significant challenges. Know the details of any limitations in your insurance plan. This can help you get necessary treatment more effectively.
People who use drugs in the United States historically have had a higher probability of being uninsured, with approximately 26% of people with a substance use disorder (SUD) uninsured compared to 20% of the general public [1].
In this article, I outline the basics for understanding your insurance benefits.
Laws Mandating Coverage
There are two major federal laws that define your right to coverage and the baseline coverage. Your individual policy still determines the specifics.
The Mental Health Parity and Addiction Equity Act (MHPAEA)
This law requires insurance plans that offer mental health and substance use disorder benefits to provide coverage that is comparable to medical/surgical coverage. For example, you can’t have higher copays or stricter limits for rehab if your plan covers hospital stays for physical illness [2] [3].
MHPAEA covers rehab services across six benefit classifications:
- Inpatient in-network/out-of-network (e.g., residential treatment, detox)
- Outpatient in-network/out-of-network (e.g., IOP, PHP, counseling)
- Emergency care (e.g., crisis stabilization),
- Prescription drugs (e.g., MAT like buprenorphine)
Examples include medically necessary inpatient rehab for SUD withdrawal, outpatient therapy sessions, partial hospitalization, and intensive outpatient programs, provided they meet plan criteria comparable to physical health analogs like post-surgical recovery.
The Affordable Care Act (ACA)
This law classifies addiction and mental health treatment as one of the 10 essential health benefits. The ACA requires Marketplace, Medicaid expansion, Medicare, and most private plans to cover substance use disorder (SUD) services, including:
- Detox,
- Inpatient rehab
- Outpatient programs: Intensive Outpatient (IOP) and Partial Hospitalization (PHP)
- Counseling
- Medication-assisted treatment (MAT)
Inpatient detox/hospitalization is covered by Medicare Part A. Outpatient and partial hospitalization are covered by Part B. In expansion states (states that expanded Medicaid under the Affordable Care Act to cover adults earning up to 138% of the federal poverty level), Medicaid often includes MAT with minimal copays.
Most major insurers provide broad access. Specifics vary by plan and state.
Coverage Prerequisites
Different plans may have varying copays, deductibles, and coverage limits, leading to significant confusion among patients. Patients may underestimate potential costs associated with facility types; for instance, a low co-pay in one setting might lead to higher bills in another [4].
Services qualify if they are considered medically necessary. However, plans may apply nondiscriminatory limits like prior authorization or network requirements, as long as these match medical benefits.
MHPAEA does not mandate offering rehab. But it does prohibit stricter financial, quantitative, or non-quantitative restrictions on substance abuse services versus medical ones.
However, studies suggest that the promise of the ACA and parity laws to increase access to SUD treatment has only partially been realized and that there are many differences between states. More reform is needed to make substance abuse treatment accessible to all who need it. [1].
What “Coverage” Actually Means: Key Terms & Variables
It’s important to know your insurance structure benefits.
Type of Facility & Program
- Inpatient/Residential vs. Outpatient (PHP/IOP): Coverage levels differ. They often require justification for 24/7 care.
- In-Network vs. Out-of-Network: In-network providers reduce your cost significantly.
Core Insurance Concepts
- Deductible: You pay this amount before insurance starts sharing the cost.
- Copay/Coinsurance: You pay this share of the cost after the deductible (e.g., $50/session or 20% of the cost).
- Prior Authorization: You need the insurer’s pre-approval for treatment.
- Medical Necessity: The treating provider must demonstrate that the chosen level of care is clinically necessary.
Length of Stay
- Coverage is often approved in segments (e.g., 7-10 days at a time). Continued care requires ongoing reviews and proof of progress.
Common Limitations
- Plans may impose prior authorizations, network restrictions (in-network preferred), or caps on the number of days or visits. Out-of-network care leads to higher costs or denials.
- Residential treatment is often excluded under standard Medicare.
- Some states limit Medicaid outpatient sessions.
- Appeals are possible for denials, based on medical necessity.
A Step-by-Step Guide to Verifying Your Benefits
Don’t guess about your coverage. It’s important to gather all the correct information.
Step 1: The Confidential Phone Call
- Call the member services number on your insurance card with your ID/group number.
- Have specific codes ready if possible
Step 2: Let the Rehab Center Help
Most reputable treatment centers have admissions teams or verification specialists who will call your insurance on your behalf, for free, to get a detailed breakdown of benefits.
- They will provide preauthorization and out-of-pocket estimates like deductibles/copays.
- Document the names and details of the provider in case you need to appeal.
Step 3: Essential Questions to Ask Your Insurer
If you call the insurance company directly, then ask these questions:
- What are my in-network benefits for inpatient residential and outpatient treatment?
- What is my deductible, and how much has been met this year?
- What are my copay or coinsurance amounts for these services?
- What is the prior authorization (verification of benefits) process for rehab admissions?
Step 4: Out-of-Pocket Costs
- You will likely have deductibles and copays (e.g., 20% under Medicare Part B) or coinsurance after meeting certain thresholds. Depending on the plan, this can potentially add thousands of dollars to your cost.
- HMO (Health Maintenance Organization) plans limit out-of-network, while PPOs (Preferred Provider Organization) offer flexibility at higher premiums.
- If you are uninsured, state-funded options or sliding-scale programs help.
What If I’m Denied Coverage? Understanding Appeals
A denial is not the final word; it’s the start of an appeals process. Denials often happen due to paperwork errors or lack of documented “medical necessity” [4] [5].
- Work with your treatment provider. They can justify the need by submitting additional clinical information (e.g., therapy notes, assessments).
- Appeal formally to your insurance company. Be persistent.
- If you believe the denial is based on unfair limitations, mention your rights under MHPAEA [3].
To file a parity complaint for denied rehab coverage under MHPAEA:
- Complete the plan’s internal appeal process.
- Then submit to the appropriate federal or state regulator based on your insurance type.
Internal Appeal Steps
- Request from your insurer the written reason for the denial, the medical necessity criteria for mental health or substance abuse treatment, medical/surgical benefits, and NQTL details.
- Submit an appeal. Reference the parity violations with a provider’s medical necessity letter comparing restrictions (e.g., prior authorization for rehab vs. surgical recovery), clinical records, and evidence-based guidelines.
- Monitor the deadlines, typically 180 days for post-service claims. Follow up as needed.
External Complaint Filing
- For fully insured plans, contact your state insurance department (find via NAIC.org).
- ERISA self-insured employer plans go to the U.S. Department of Labor (dol.gov/agencies/ebsa)
- Federal employee plans go through HHS.
- Medicaid goes to your state Medicaid agency.
Additional Support
- For appeals, use free templates from ParityTrack or CounterForce Health. They claim 70-80% success rates.
- Consult advocates like the NAMI Helpline or state attorneys general for assistance; external reviews may follow exhausted appeals.
Key Takeaways
- Financial concerns should not deter you from seeking life-saving help. Coverage is available.
- Use the steps outlined here to verify your benefits today.
- Reach out to a treatment center for a confidential consultation and insurance check—it’s the most concrete way to move forward.
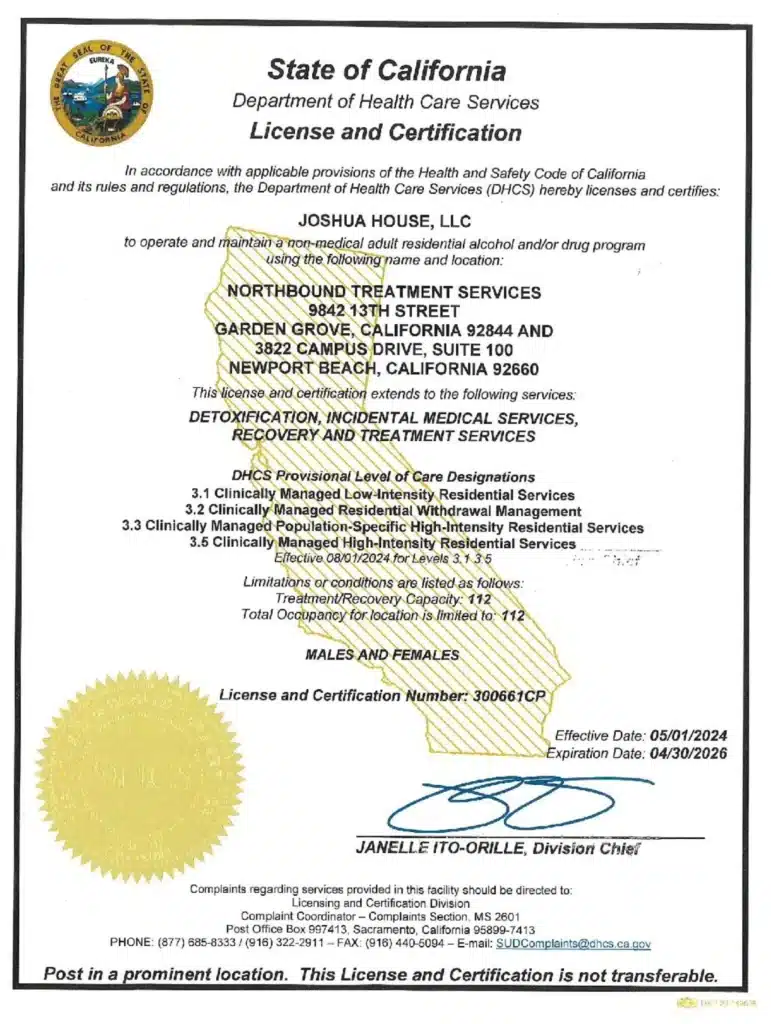
Why Choose Northbound Treatment Services?
At Northbound, we have extensive experience helping patients overcome their substance abuse addictions, and we have a Christian faith-based track for those wishing to participate.
We offer a wide range of evidence-based therapies, counseling, and trauma-informed support to assist you in your healing. We personalize each treatment plan around the needs of our patients.
The first steps are detoxification and stabilization, under 24-hour medical supervision in our Withdrawal Management center for whatever time you may require.
Our inpatient residential program offers 24/7 live-in treatment for substance abuse. Our outpatient treatment provides a flexible step-down from our residential program, allowing you to live at home and participate for several hours a day.
For more than 30 years, Northbound Treatment Services in California has been at the forefront of providing lifesaving, compassionate residential care and specialized services to help people from all walks of life feel better, discover themselves, and live free from addiction.
We have facilities located throughout California to help guide you on your recovery journey. Reach out to our admissions team now.
Sources
[1] Dickson-Gomez, J., et al. (2022). Insurance barriers to substance use disorder treatment after passage of mental health and addiction parity laws and the affordable care act: A qualitative analysis. Drug and alcohol dependence reports, 3.
[2] Medicaid.gov. nd. Parity.
[3] National Alliance on Mental Illness. nd. What is Mental Health Parity?.
[4] Valley Forge. nd. Insurance Coverage Struggles for Rehab.
[5] Tal Begin Anew. nd. Problems Getting Insurance Coverage for Drug Rehab? You Are Not Alone.
Author
-

President, CEO & Founder at Northbound Treatment Network
Paul Alexander is the CEO, President & Founder of Northbound Treatment Network in Newport Beach, California. He believes wholeheartedly in transformational leadership, organizational health and effective, fully integrated substance use disorder and mental health treatment. With over 27 years of experience in behavioral healthcare, Paul has extensive knowledge of “in vivo” treatment modalities, clinical development, operations, strategy, marketing and financial planning. He has been widely recognized for his development of collegiate-based residential treatment programs for students in recovery and authored a research study at The University of California confirming this modality’s effectiveness.
Paul’s comprehensive professional experience, willingness to innovate, and emphasis on organizational health are vital factors in Northbound’s continued success. Paul received his Certified Addiction Treatment Specialist training at Saddleback College in Mission Viejo, CA, and was awarded Outstanding Alumni Service Award in 2002. Paul holds a Bachelor of Arts degree in Criminology, Law and Society, Summa Cum Laude, from University of California, Irvine, and a Juris Doctorate degree from Loyola Law School of Los Angeles. Paul currently serves on The National Association of Addiction Treatment Providers (NAATP) board. In addition, he serves on The Family Recovery Foundation board and The CarePossible board in Orange County; both organizations are committed to raising funds for family recovery and treatment for former military personnel. Paul is in recovery himself and lives in Orange County with his wife Silvana and his two young sons, Noah and Dean.